 USE OF EMPLOYMENT AND SUPPORT ALLOWANCE INFORMATION IN CLAIMS FOR DISABILITY LIVING ALLOWANCE
USE OF EMPLOYMENT AND SUPPORT ALLOWANCE INFORMATION IN CLAIMS FOR DISABILITY LIVING ALLOWANCE
A Handbook for Decision Makers
Forward
This handbook has been prepared by the Department’s Health, Work and Wellbeing Directorate. It considers how Disability Living Allowance (DLA) Decision Makers (DMs) can use the information obtained in assessing Employment and Support Allowance in determining DLA benefit entitlement.
________________________________________________________________________________
Employment and Support Allowance (ESA) has been introduced in October
2008, for new claimants, and will replace Incapacity Benefit and Income
Support paid on grounds of incapacity. Analysis has shown that a large
percentage of DLA claimants have a current or recent claim to incapacity
benefit. Valuable information relating to the customer’s medical condition and
functional limitations will be available in the documentation used to evaluate
the ESA claim. Using this information may save the customer from having to
undergo an examination in connection with their DLA claim, and reduce the
need to obtain further clinical information from the customer’s doctor or
another health care professional (HCP).
Section 1 – Background
1 The Employment and Support Allowance has been designed to enable
people to achieve their full potential through work and to help them to gain
independence from benefits. It will focus on what the person can do rather
than what they cannot do. The overarching principle is that everyone should
have the opportunity to work, and that people with an illness or disability
should get the help and support needed for them to engage in appropriate
work.
2 ESA requires all but those patients with the most severe illnesses or
disabilities to engage in a programme of work focused interviews and develop
a work related action plan as a condition of receiving the allowance.
3 The assessment process for deciding entitlement to benefit and rate of
benefit paid is the Work Capability Assessment (WCA). The Work Capability
Assessment replaces the Personal Capability Assessment (PCA) used to
determine entitlement to Incapacity Benefit. Within the WCA, there are a
number of assessments:• Limited Capability for Work Related Activity (LCWRA) – This
assessment aims to identify, through a series of descriptors, customers
with the most severe illnesses or disabilities. These customers will
identified as members of the Support Group of ESA and will not have
to engage in work – focused interviews as a condition of receiving
benefit.
• Limited Capability for Work Assessment (LCW) – This aims to identify
those people who currently have a limited capability for work, but who
would benefit from assistance and support with work and health related
activity to maximise their full potential. This part resembles the PCA,
but the descriptors have be reviewed and revised for both physical and
mental functional capabilities. The report (ESA 85) generated from this
part of the assessment will available to the DLA Decision Maker.
• Work Focused Health related Assessment (WFHRA) – This part
comprises an interview with a healthcare professional to explore the
customer’s views about moving into work and any health related
interventions that would facilitate this.
Section 2 – The Work Capability Assessment
1 The Work Capability Assessment will be applied to all customers within the
first thirteen weeks of claiming Employment and Support Allowance. It will
assess, for the purposes of determining entitlement, whether a customer can
be considered to have limited capability for work. It will also help determine
the rate at which ESA is awarded from week fourteen.
2 The Work Capability Assessment looks at the effects of any illness or
disability on the customer’s ability to carry out a range of everyday work
related activities. The outcome of WCA determines if a person has limited
capability for work. If a customer does not have limited capability for work they
will be provided with advice about registering for employment and claiming
other benefits.
3 The following Activities are evaluated in the assessment:
Physical assessment
4 There are eleven Activities relevant to the physical assessment:
• Walking with a walking stick or other aid if such aid is normally used;
• Standing and sitting;
• Bending or kneeling ;
• Reaching;
• Picking up and moving or transferring by the use of the upper body and
arms;
• Manual dexterity;
• Speech;
• Hearing with a hearing aid or other aid if normally worn; • Vision including visual activity and visual fields, in normal daylight or
bright electric light, with glasses or other aid to vision if such aid is
normally worn;
• Continence; and
• Remaining conscious during waking moments.
Mental, cognitive and intellectual function assessment
5 There are ten Activities relevant to the mental, cognitive and intellectual
function assessment:
• Learning or comprehension in the completion of tasks;
• Awareness of hazards;
• Memory and concentration;
• Execution of tasks;
• Initiating and sustaining personal action;
• Coping with change;
• Getting about;
• Coping with social situations;
• Propriety of behaviour with other people; and
• Dealing with other people.
6 For each of the Physical and Mental Health Activities there is a set of
statements ranked in order of functional restrictions known as the descriptors.
They describe different levels of functional limitation.
7 Each descriptor that is relevant to a customer’s illness or disability has a
score.
For example, Walking is defined as ‘Walking with a stick or other aid if such
aid is normally used’ and there are six descriptors:-
• Cannot walk at all (score 15)
• Cannot walk more than 50 metres on level ground without repeatedly
stopping or severe discomfort (score 15)
• Cannot walk up or down two steps even with the support of a handrail
(score 15)
• Cannot walk more than 100 metres on level ground without stopping or
severe discomfort (score 9)
• Cannot walk more than 200 metres on level ground without stopping or
severe discomfort (score 5)
• None of the above apply (score 0).
8 Getting about is an example of one of the Mental function Activities, and
there are five descriptors:-
• Cannot get to any specified place with which the customer is, or
• would be, familiar (score 15)
• Is unable to get to a specified place with which the customer is • familiar, without being accompanied by another person on each
occasion (score15)
• For the majority of the time is unable to get to a specified place with
• which the customer is familiar without being accompanied by another
• person (score 9)
• Is frequently unable to get to a specified place with which the
• customer is familiar without being accompanied by another person
(score 6)
• None of the above apply ( score 0)
Combinations of disabilities
9 Many people may have more than one disability. The assessment therefore
includes a means of taking into account the combined effects of different
disabilities. For example, if a customer could walk 50 metres or more but
could not walk 200 metres without stopping or severe discomfort, this by itself
would score 6. However, if they also had difficulties with ‘Manual dexterity’
such as cannot physically use a pen or pencil, this would score an additional
9. Any further score awarded in respect of functional limitation caused by a
mental health disorder is added to reach the total. If a customer is awarded a
score of 15 or more, they will be entitled to Employment and Support
Allowance and be considered as having limited capability for work.
Section 3 – Overview of the Claim Process
1 In the majority of cases the initial claim for ESA is made via Jobcentre Plus
by telephone. When someone becomes entitled to ESA they enter a thirteen
week assessment phase. If it is apparent at this initial stage that the customer
is terminally ill (Special Rules), benefit is paid without the need to undergo
further assessment. Some other customers, for example, people receiving
chemotherapy or regular haemodialysis, will also be considered as having
limited capability for work without taking part in the full Work Capability
Assessment.
2 If a customer is not identified as having limited capability for work or limited
capability for work-related activity at the preliminary stage, they are asked to
complete questionnaire ESA 50 providing details of their illnesses and
functional limitations. The claim is assessed by Medical Services using
evidence in the ESA 50 questionnaire, medical certification and any further
medical evidence requested by Medical Services. Medical Services will
determine if the person fulfills the criteria as having limited capability for work
or entry into the Support Group of ESA (see below) without having to undergo
further assessment including medical examination.
3 People eligible for inclusion in the Support Group are those who have the
most severe illnesses and disabilities, including terminal illnesses. Customers
fulfilling the criteria for the Support Group are treated as having limited
capability for work and for work related activity. They are assessed in respect
of eleven Activities, and Medical Services will advise the ESA DM on report ESA 85A if at least one of the descriptors applies to the customer. The eleven
Activities are:
• Walking or moving on level ground;
• Rising from sitting and transferring from one seated position to another;
• Picking up and moving or transferring by the use of the upper body and
arms;
• Reaching;
• Manual dexterity;
• Continence;
• Maintaining personal hygiene;
• Eating and drinking
• Personal action; and
• Communication.
Full details of the Activities and the descriptors can be found in Appendix A.
4 Customers not in the Support Group or having LCW/LCWRA are called for
assessment, when the medical examination is recorded on form ESA 85, and
a WFHRA is carried out. The medical report ESA85 provides medical
evidence and information that is likely to be useful to the DLA DM. It may,
however, become apparent at this assessment that the customer has a
severe illness or disability such that they fulfill the criteria for the Support
Group, and the ESA DM is advised accordingly.
5 On the basis of the information in report ESA85 the Decision Maker
determines whether the customer has limited capability for work. The
customer is considered as having limited capability for work if he:
• scores 15 points in respect of the physical descriptors; or
• 15 points in respect of the Mental Function descriptors; or
• 15 points in respect of the descriptors in a combination of mental
function and physical descriptors).
In both the physical and mental function categories, the highest descriptors in
any functional area attract 15 points and the lowest descriptors have a 6 point
value. A customer may reach the prescribed degree of disability to be
considered as having limited capability for work, if they are awarded the
highest descriptor in any one physical or mental function category or through
a combination of lower scoring descriptors in a number of functional areas.
6 Customers reaching the threshold for limited capability for work will be
required to attend a series of six Work Focussed Interviews with their
Personal Adviser at Jobcentre Plus. During these sessions an agreed action
plan of activity will be drawn up to help the customer with a potential return to
work.
Section 4 – Overview of how the Work
Capability Assessment can be used in DLA1 The medical report form ESA85 is completed as part of the assessment of
the customer at the Medical Examination Centre. It contains valuable
information including factual information about the medical condition and the
customer’s functional limitations.
2 These include:
• Diagnoses;
• Medication and any side effects;
• History of condition;
• Recent hospital treatment;
• Description of daily activities and how these relate to function (typical
day interview);
• Clinical findings;
• Observed behaviour; and
• Advice regarding functional limitations in the prescribed Activities.
The specific features of the ESA 85 report that are of greatest use to the DLA
DM are described in detail in subsequent sections.
2 As explained in Section 3 above some customers with the most severe
illnesses and disabilities that fulfil the criteria for inclusion in the Support
Group may be identified at the medical examination. The ESA DM will be
advised of this in an additional report ESA 85A, and this report may also be
available to the DLA DM in a small number of cases. Its potential use to the
DLA DM will be described later in this guidance.
Section 5 – What happens at the Medical
Assessment
Approved disability analyst
1 The medical assessment process as a whole differs in many respects from
traditional history taking and examination that occurs in the general practice or
hospital setting. It entails bringing together information gained from
observation, questionnaire, medical evidence and examination in order to
reach an accurate assessment of the customer’s functional restrictions. The
assessment is carried out by an Approved Disability Analyst.
2 All health care professionals who give advice relating to Employment and
Support Allowance must be approved by the Secretary of State for Work and
Pensions. The approved disability analyst may be a registered medical
practitioner, registered nurse, registered occupational therapist or registered
physiotherapist. Approval involves attendance at a prescribed training course,
written assessment of medical knowledge, successful completion of the
stages of the approval process, and ongoing demonstration that the work
being carried out meets a satisfactory standard including attendance at future
professional educational events.3 Examining Medical Practitioners who carry out DLA/AA assessments
undergo a similar process of training and monitoring, and are approved as
disability analysts by the DWP Secretary of State.
4 The approved disability analysts who undertake the WCA are employed by
Medical Services. Their role is different from the clinical role of the GP or
hospital specialist, which is to diagnose and treat the patient. The clinician is
an expert in arriving at a diagnosis, using physical examination and special
investigations in combination with detailed knowledge of treatments.
Clinicians are not experts in assessment of disability, since they have not
received training in determining the disabling effects of medical conditions on
a person’s every day life and activities. See table at Appendix D.
5 The medical disability analyst provides the Decision Maker with justified
advice that takes into account the clinical history, examination, observed
behaviour and their knowledge of the disabling effects of the medical
condition(s). The advice is consistent, evidence based and in accordance with
the legislative criteria of the benefit.
6 There are four stages in the ESA LCW/LCWRA Assessment. These are:
• Reading the documents;
• Interviewing the customer;
• Examining the customer; and
• Completing the medical report.
Reading the Documents
7 In preparation for the interview the disability analyst reads the documents in
the file. All the medical evidence is considered, including medical certificates,
factual reports, any previous examination and other documents, including
Tribunal documents. Particular attention is paid to the current customer
questionnaire (ESA 5O).
8 When the disability analyst has read the documents, he or she usually goes
to meet the customer in the waiting room, and accompanies them from the
waiting room to the interview/examination room. In addition to being a natural
courtesy it helps to put the customer at ease, and allows the disability analyst
to observe the customer’s activities outside the examination room. The
disability analyst will observe how the customer rises from the chair, walks
etc.
Interviewing the Customer
9 The nature of the interview differs materially from the traditional consultation
in clinical practice. The aim of the traditional interview is to arrive at a
diagnosis and treat the patient. In the LCW/LCWRA interview, the disability
analyst gathers information to assess the claimant’s abilities in all of the
relevant functional areas. A concise and relevant medical history is included.10 One of the most important aspects of the interview is the Typical Day
enquiry. This is a record of the customer’s everyday life including a factual
description of how the medical condition affects their day-to-day activities. The
disability analyst records the account in note form; it is not a statement.
Experience shows that Decision Makers find this section of the report
particularly helpful.
The examination
11 When the interview has been completed, the disability analyst seeks the
customer‘s consent for physical examination of the relevant functional areas.
The granting of this consent is noted in the report. Mental state examination
and completion of the Mental Function assessment is carried out where there
is evidence of mental disease or disablement (mental illness, learning
disabilities, cognitive impairment or sedative medication).
12 Informal observations of the customer are also made during the entire
period of customer contact and incorporated into the report. The disability
analyst looks for consistency when evaluating the informal observations, the
clinical examination findings, the clinical history, and the analyst’s knowledge
of the disabling effects of the customer’s medical condition(s).
Completing the medical report form ESA 85
13 The disability analyst completes the medical report ESA 85 choosing and
justifying the relevant descriptors. In the majority of claims a computerised
version of the report using Logic integrated Medical Assessment (LiMA) is
provided for the Decision Maker.
14 Where the disability analyst’s choice of descriptor differs from the
customer’s stated level of disability, the disability analyst provides justified
advice to the Decision Maker supported by the evidence to explain why their
opinion, rather than the customer’s, should be accepted.
15 If the customer has a severe illness or disability such that they fulfil the
criteria for inclusion in the Support Group both the examination and the report
completion may be curtailed. Additional information is then provided on form
ESA 85A – see Section 16.
16 Report completion may also be curtailed if the customer has high levels of
functional restriction in a number of areas i.e. the highest-ranking descriptors
are applicable for a number of Activities. Under these circumstances LiMA
invites the author to provide the most detailed justification in the most highly
scoring activities, and less information is provided about other Activities.
17 The time spent with the customer is recorded on the report, and includes
the time from greeting the customer in the waiting room until the end of the
interview and examination. The additional time that it takes to complete the
report is recorded. The time spent on the medical assessment will depend on the complexity of the case. It is estimated that the overall time to complete the
WCA will be between 75 and 90 minutes.
Section 6 – Choosing descriptors
1 The disability analyst selects their choice of descriptor in each of 11 physical
functional areas (Activities), and if relevant to the case, in each of 10 mental
function areas.
2 The choice of the most appropriate descriptor in the relevant functional
areas depends upon consideration of all the medical evidence, the customer
interview, the medical examination, and the disability analyst’s medical
knowledge of the likely effects of the disabling condition.
3 For each of the mental, physical and sensory functional areas (Activities)
the disability analyst chooses only one descriptor, and this is the descriptor,
which reflects the customer’s level of functioning most of the time, taking into
account such factors as pain, stiffness, response to treatment and variability
of symptoms. This ensures that the opinion is not just a “snapshot” of the
customer on the day of examination, but reflects their functional ability over a
period of time. See below for more detail.
4 In certain functional areas, the descriptors do not conform to a simple
hierarchical progression. In these areas the descriptor chosen is that which
most accurately reflects the highest level of disability experienced by the
claimant. For example, in the functional area of Continence, when a customer
loses control of bladder so that the person cannot control the full voiding of
the bladder at least once a month and loses control of bowels so that the
person cannot control the full evacuation of the bowel occasionally, the latter
is selected, as it is the “higher” descriptor.
5 If the disability analyst‘s opinion on the level of functional restriction in any
Activity differs from that of the customer, as indicated on the ESA 50
questionnaire or as described at interview, the disability analyst provides a full
justification for their opinion. The justification of descriptor choice is supported
by information from the clinical history, activities of daily living, observation of
the customer, and clinical examination findings.
6 A number of functional activity areas on the ESA 85 are linked e.g. walking,
standing and sitting, and bending and kneeling, and justification for these
group of functional areas are entered together in the appropriate boxes.
Clinical details may be cross-referred to other relevant linked groups.
Evidence should be consistent so that contradictions do not in different
sections of the report. Any apparent contradictions are explained such that the
Decision Maker is able to understand that two pieces of evidence, which at
first sight appear contradictory, are in fact compatible with one another.
7 On occasions the disability analyst will choose a “None of the above apply”
descriptor, even though some disability has been identified. In these circumstances the level of functional restriction is not severe enough to reach
the lower threshold; i.e. the penultimate descriptor. For example, the customer
may have indicated that they have difficulty with walking, but the evidence
from the assessment shows they only experience significant discomfort after
walking at a reasonable pace for 20 minutes (i.e. they can manage over 800
m).
Section 7 – Variable and fluctuating conditions
1 The disability analyst is required to provide the Decision Maker with medical
advice on the most appropriate level of functional ability in each Activity. In
doing so they must take into account a number of factors including:
• Any fluctuations in the medical condition i.e. how the condition changes
with time.
• The variation of functional ability i.e. how the person’s functional ability
changes over time and in relation to changes in the underlying medical
condition.
• Any pain that results from performing the activity.
• The ability to repeat the activity.
• The ability to perform the activity safely.
2 The disability analyst’s choice of descriptors reflects what the person is
capable of doing for most of the time. In other words, could the person
normally carry out the stated activity when called upon to do so?
3 For conditions that vary from day to day a reasonable approach would be to
choose the functional descriptors, which apply, for the majority of the days.
(N.B some of the Mental Function descriptors specify frequency of limitation
and are considered individually).
4 In some cases the disability analyst has to consider whether the claimed
level of disability on ‘good’ and ‘bad’ days is likely to be consistent with the
clinical picture presented, the diagnosis and the overall pattern of daily
activity. The disability analyst provides the DM with advice on:
• The customer’s functional limitations on the majority of the days.
• The limitations found on the remaining days where the customer’s
condition is worse or better, with an indication of the frequency with
which these days arise.
5 For conditions that vary through the day the choice of descriptor should
reflect that level of activity, which can be performed for a reasonable
continuous period within the day.
6 If a person cannot repeat an Activity with a reasonable degree of regularity,
and certainly if they can perform the Activity only once, then they are
considered unable to perform that Activity. 7 The customer must be able to undertake the Activity safely. If a person with
vertigo is physically able to bend to touch his knees but in so doing falls over
due to giddiness, then he is considered incapable of performing that Activity.
8 The Activities do not have to be performed without any discomfort or pain.
However if the customer cannot perform an Activity effectively because of
pain they are considered incapable of performing that Activity.
9 When considering the effects of pain, the predictability of onset and the
effectiveness of treatment are taken into account. Pain that starts without
warning and requires analgesia is very different from predictable angina of
effort that can be forestalled, or rapidly relieved, with appropriate treatment
(e.g. GTN spray).
10 Breathlessness is an important symptom, because it is not specifically
reflected in many of the descriptors, but it may contribute significantly to
disability, for example, in relation to walking. Therefore, a customer who
experiences significant breathlessness when carrying out an activity should
be scored as if the activity cannot be undertaken.
11 The disability analyst will advise on the consistency of the variable factors
with the diagnosis and with the stage reached by the disease, and with the
customer’s lifestyle.
For example, the medical certification says the customer has mechanical back
pain, and on examination there is no lumbar spine abnormality. The customer
says that on one day a week his back is so bad that he has to stay in bed.
This degree of variability is very unlikely; mechanical back pain does not
normally vary to this extent.
Section 8 – Physical and Sensory Activities
Eleven specified physical Activities are assessed. These are grouped together
as follows:
Lower Limb – Activities 1, 2 and 3
• Walking;
• Standing and sitting; and
• Bending and kneeling.
Upper Limb – Activities 4, 5 and 6
• Reaching;
• Picking up and moving or transferring by the use of the upper body and
arms; and
• Manual dexterity.
Special functions – Activities 7, 8 and 9• Vision;
• Speech; and
• Hearing.
Continence – Activities 10 (a), 10 (b) and 10 (c)
Remaining conscious – Activity 11
Section 9 – Mental Health Activities
1 This part of the ESA 85 report is completed when a specific mental disorder
has been diagnosed, or where there is any condition, that could be mental,
physical or sensory, that results in the cognitive or intellectual impairment. In
addition the assessment is undertaken in the following circumstances:
• where the customer is taking any medication which affects cognitive
abilities to a degree that causes mental impairment;
• where there is evidence of an alcohol /drug dependency problem which
has resulted in mental impairment;
• where there is evidence of a physical or sensory disability such as
tinnitus or chronic fatigue that may impact on mental function;
• where there is evidence of learning disability;
• where there is evidence of acquired brain injury; and
• where there is a previously unidentified mild or moderate mental
function problem identified during the LCW/LCWRA assessment.
2 If the disability analyst does not consider that it is necessary to apply the
mental function assessment, they are required to justify this. This is likely to
be the case where there is no recent history of diagnosis or treatment of
mental illness, and where there is no evidence at the assessment of any
condition, diagnosed or apparent, that is likely to impair mental function.
3 There are ten Activities (functional categories) that are addressed in the
ESA LCW/LCWRA mental assessment. These categories cover a number of
areas relevant to those with a specific mental illness, or cognitive or
intellectual impairment. These categories are grouped together in the ESA 85
report as follows:-
Understanding and focus (Activities 12, 13, 14, 15 and 16)
• Learning or comprehension in the completion of tasks;
• Awareness of hazard;
• Memory and concentration;
• Execution of tasks; and
• Initiating and sustaining personal action.
Adapting to change (Activities 17, 18 and 19)
• Coping with change; • Getting about; and
• Coping with social situations.
Social Interaction (Activities 20 and 21)
• Propriety of behaviour with other people; and
• Dealing with other people.
4 In the ESA 85 report a structured Mental State Examination is provided by
the disability analyst from which he or she draws evidence to support their
choice of descriptors. Information is recorded under the following headings:
• Appearance;
• Behaviour/volition;
• Conversation;
• Cognition – general;
• Cognitive tests – informal;
• Cognitive tests – formal;
• Insight;
• Addictions; and
• Involuntary movements.
Section 10 – Differences between IB 85 and ESA
85
1 As described at the beginning of this guidance the WCA has been designed
to focus on a person’s capabilities with an emphasis on what they can do
rather than what they cannot. Both the physical and mental Activities have
modified so that they reflect the type of work related activities relevant to the
modern work place. The physical Activities recorded in the IB 85 have been
extensively revised for ESA. Changes include removal of some Activities,
amalgamation of others, inclusion of new descriptors and revision and
deletion of existing descriptors. The descriptor scores have also been revised
to reflect the aims of the new assessment and benefit.
2The table at Appendix B summarises the main differences in the physical
assessment between the ESA 85 report and the IB 85.
3 The mental health questionnaire found in the IB 85 has been replaced by
the new ESA mental function assessment. There are no longer 25 descriptors
presented as a series of questions requiring a yes or no answer. In the ESA
85 there are 10 new mental function Activities, each of which has a number of
ranked descriptors. This mirrors the format of the physical assessment, and
the disability analyst chooses a descriptor for each Activity, and the descriptor
is scored.
Section 11 –The ESA 85 report and its relevance
to the DLA Decision MakerThe information in the ESA 85 presented under the following headings:
1 A list of medical conditions, previously diagnosed, found at the medical
assessment or reported by the customer.
2 Medication, dosage and the reasons for its use.
3 Side effects of the medication as reported by the customer with the disability
analyst’s comment on their functional relevance.
4 History of the medical conditions and how they affect function.
5 Record of any hospital treatment and tests within the last yea.r
6 History of any specific therapy for mental health problems with the past 3
months.
7 Social and occupational history including the reason for leaving work.
8 Description of a typical day.
9 Medical opinion – Physical. This section records the disability analyst’s
choice of descriptors for the eleven physical functional areas (Activities). The
Activities are grouped together under a number of headings i.e. Lower limb,
Upper limb, Special senses, Continence and Remaining Conscious. Within
each of these groupings the medical evidence used to justify the choice of
descriptor for each Activity is presented under four sub-headings:
• Prominent features of functional activity relevant to daily living;
• Behaviour observed during assessment;
• Relevant features of clinical examination; and
• Summary of functional ability.
10 Mental Function – the disability analyst indicates if the mental function
assessment has been applied. If not, an explanation why it has not been
applied is recorded.
11 Medical opinion – Mental function. This section records the disability
analyst’s choice of descriptors for the ten mental functional areas (Activities).
The Activities are grouped together under three headings i.e. Understanding
and focus, Adapting to change and Social Interaction. Within each of these
groupings the medical evidence used to justify the choice of descriptor for
each Activity is presented under three sub-headings:
• Prominent features of functional activity relevant to daily living;
• Relevant features of clinical examination and
• Summary of functional ability.
12 Advice on Exceptional Circumstances (also known as non-functional
descriptors). These relate to a small number of severe medical conditions that do not result in a score that is sufficient to reach the benefit threshold of 15,
but would render the customer unfit for work. Since such cases do not usually
have significant functional restrictions, it is unlikely that the information
pertaining to this category will be of direct relevance to the DLA DM.
13 Limited Capability for Work Related Activities. In this section the disability
analyst gives an opinion as to why the customer does not meet any of the
descriptors for the Limited Capability for Work- Related Activity. i.e. fulfill the
Support Group criteria. This is the most likely outcome in the majority of
cases, and this information is not likely to be of direct use to the DLA DM.
14 In a small number of cases additional information will be available on
report ESA 85A for customers who meet the criteria for the Support Group.
This information may be useful to the DLA DM and this is discussed below in
section 16.
15 Advice on prognosis (when likely to be a significant improvement in
function)
16 Summary of medical examination findings (physical and/or mental).
Section 12 – The Physical Assessment and its
use in DLA
In this section detailed information about each of the Physical Activities and
the ranked descriptors is provided. An explanation of the scope of each
Activity is combined with notes about the type of specific evidence that the
disability analyst takes into account in making their descriptor choice. For
each Activity additional guidance on how the ESA 85 report may be used to
evaluate care and mobility (DLA considerations) is provided.
Lower Limb function
• walking
• standing and sitting
• bending and kneeling
Upper Limb
• reaching
• picking up
• manual dexterity
Sensory• speech
• hearing
• vision
Continence
Remaining conscious
Walking – Activity 1
Walking with a walking stick or other aid if such aid is normally used.
Descriptors
W (a) Cannot walk at all
.
W (b) Cannot walk more than 50 metres on level ground without repeatedly
stopping or severe discomfort.
W(c) Cannot walk up or down two steps even with the support of a handrail
W (d) Cannot walk more than 100 metres on level ground without stopping or
severe discomfort.
W (e) Cannot walk more than 200 metres on level ground without stopping or
severe discomfort.
W (f) None of the above apply.
Scope
1 This Activity is intended to reflect the level of mobility that a person would
need in order to be able to move reasonably within and around an indoor
environment. It is intended mainly to apply to lower limbs impairments;
however walking ability may also be restricted by limited exercise tolerance
due to respiratory or cardiovascular disease. Conditions affecting upper limb
function i.e. ability to use a stick, are not taken into consideration.
2 Walking is bipedal locomotion, that is, movement achieved by bearing
weight first on one leg and then the other. Those who are wheelchair
dependant or can only swing through on crutches do not fulfil this definition,
and therefore fall within descriptor W (a).
3 When estimating the distances over which a customer can walk, the
disability analyst takes account of brief pauses made out of choice rather than necessity. The end point is when the customer cannot reasonably proceed
further because of substantial pain, discomfort, or distress.
4 Descriptor W(c) also reflects a severe limitation of stair climbing. This may
be caused by severe lower limb impairments or breathlessness. It should be
noted that the descriptor indicates inability to perform this task even if holding
on to a handrail(s). Therefore the individual’s abilities are considered within
the context of a handrail being present. This activity reflects a test of walking
up or down 2 steps, not of whether one hand or two hands is needed for
support while doing so. Therefore a person who can manage the two steps
with support of two
5 The disability analyst notes any restrictions due to breathlessness or
angina, as well as any relevant musculoskeletal problems. If a particular
descriptor activity could only be performed by inducing significant
breathlessness or distress, a higher descriptor is chosen.
6 Walking may occasionally also be affected by disturbances of balance due
to for example, dizziness or vertigo. The effects of any such condition will be
noted and full details given in the medical report.
Details of daily living
7 The disability analyst considers the customer’s walking ability in relation to:
• Mobility around the home; and
• Shopping trips, exercising pets.
8 The report may include details of distances walked and how long it takes the
customer to walk any particular distance; whether the customer needs to stop,
and if so how often, and for how long? Normal walking speed is 61-90m/min;
a slow pace would be around 40-60m/min and a very slow pace less than
40m/min.
9 The method of travel to the examination centre is relevant. The disability
analyst is likely, from local knowledge, to be aware of the distance from the
bus station to the examination centre and may record the distance, time
taken, the number of rests required, and the lengths of the rest periods.
Observed behaviour
10 The disability analyst observes the customer walking from the waiting area
to the examination room, and notes their gait, pace and any problem with
balance. They will look for evidence of breathlessness caused by walking.
11 The disability analyst notes the use of any aids e.g. walking stick, and
whether their use was appropriate. They also record any assistance needed
from another person.Clinical examination
12 Restricted ability to walk will commonly be due to musculoskeletal and
neurological disorders affecting the lower limbs, and sometimes the lumbar
spine. Restrictions may also be due to diseases of the respiratory or
cardiovascular systems, with limitation of exercise tolerance as a result of
breathlessness, angina or claudication.
13 Where relevant, an appropriate assessment of the heart and lungs is
carried out, with a record of any cyanosis, dyspnoea at rest or on minimal
exertion, the presence of audible wheeze, signs of heart failure such as ankle
oedema, and the state of peripheral blood vessels. Any respiratory or
cardiovascular factors affecting exercise tolerance are taken into account
when choosing the descriptor.
14 Peak flow may be measured, if appropriate, and the recorded
measurement interpreted for the DM within the context of the other available
information. Comment on technique or effort may also be made.
DLA considerations
15 If one of the first three descriptors is chosen i.e.
W (a) Cannot walk at all.
W (b) Cannot walk more than 50 metres on level ground without repeatedly
stopping or severe discomfort.
W(c) Cannot walk up or down two steps even with the support of a handrail
it is likely that there is significant walking restriction. This will also indicate that
the person has difficulty in using stairs.
16 If descriptor W (d) is chosen Cannot walk more than 100 metres on
level ground without stopping or severe discomfort, it is unlikely that the
person is restricted in their walking to a lesser distance. If the disability analyst
judged that the person could only walk 75 metres, they would chose the
higher descriptor W(b)
17 Note that in evaluating this Activity the disability analyst takes into account
factors such as pain, fatigue, balance, gait, ability to walk at a reasonable
speed and breathlessness. If the person has severe breathlessness due to
cardiac or respiratory diseases this will be reflected in the descriptor choice,
even if lower limb function is normal.
18 The descriptor choice will be supported by the disability analyst’s own
observation of the person walking at the examination centre, and the account
of their daily activities. It is worth noting that a person who can easily manage
around the house and garden is unlikely to be limited to walking less than 200 metres; a person who can walk around a shopping centre/supermarket is
unlikely to be limited to walking less than 800 metres.
Standing and sitting – Activity 2
Descriptors
S (a) Cannot stand for more than 10 minutes, unassisted by another person,
even if free to move around, before needing to sit down.
S (b) Cannot sit in a chair with a high back and no arms for more than 10
minutes before needing to move from the chair because the degree of
discomfort experienced makes it impossible to continue sitting.
S(c) Cannot rise to standing from sitting in an upright chair without physical
assistance from another person.
S (d) Cannot move between one seated position and another seated position
located next to one another without receiving physical assistance from
another person.
S (e) Cannot stand for more than 30 minutes, even if free to move around,
before needing to sit down.
S (f) Cannot sit in a chair with a high back and no arms for more than 30
minutes without needing to move from the chair because the degree of
discomfort experienced makes it impossible to continue sitting.
S (g) None of the above apply.
Scope
1 This Activity relates to lower limb and back function. It is intended to reflect
the need to be able to remain in one place, either sitting or standing. When
standing, a person would not be expected to have a need to stand absolutely
still, but would have freedom to move around or shift position whilst standing.
S (d) “Moving between adjacent seated positions” is intended to reflect a
wheelchair user who is unable to transfer, without help, from the wheelchair.
Sitting
2 When considering sitting the following are taken into account:
• Sitting involves the ability to maintain the position of the trunk without
support from the arms of a chair or from another person.
• Sitting need not be entirely comfortable. The duration of sitting is
limited by the need to move from the chair because the degree of discomfort makes it impossible to continue sitting, and therefore any
activity being undertaken in a seated position would have to cease.
• Inability to remain seated in comfort is only very rarely due to
disabilities other than those involving the lumbar spine, hip joints and
their related musculature.
Details of daily living
3 The disability analyst considers the customer’s ability in relation to:
• Watching television (for how long at a time and type of chair).
• Other leisure or social activities, e.g. listening to the radio, using a
computer, sitting in a friend’s house, pub or restaurant, cinema,
reading, knitting.
• Sitting at meal times (which may involve sitting in an upright chair with
no arms).
• Time spent travelling in cars or buses.
Observed behaviour
4 The disability analyst records the customer’s ability to sit without apparent
discomfort within the examination centre, both in the waiting area and during
the interview, where this has been observed. The record should state the type
of chair.
Standing
5 When considering standing, it should be noted that descriptor S(a) reflects
the ability to stand without the support of another person. This reflects a very
significant level of disability in relation to standing.
6 S (e) reflects the ability to stand even with the use of aids. The ESA
regulations specify “the person is to be assessed as if wearing any prosthesis
with which [he] is fitted, or wearing or using any aid or appliance which is
normally worn or used”. So a person who can stand with the aid of two sticks
is, for the purpose of descriptor choice, able to stand.
7 The requirement to sit down suggests a greater degree of disability than
simple discomfort resulting in a need to move around. It would normally be
expected that significant lower limb problems and muscle weakness would be
present
Details of activities of daily living
8 The disability analyst considers the customer’s ability in relation to:
• Standing to do household chores such as washing up or cooking.
• Standing at queues in supermarkets or waiting for public transport,
standing and waiting when collecting a child from school. • Standing to watch sporting activities.
The report should include comments on the length of time the customer
stands during any such activities.
Observed behaviour
9 It is usually only possible to observe the customer standing for short periods
of time during the assessment and the report should reflect this, e.g.
“I observed him standing for 3 minutes only during my examination of his
spine but he exhibited no distress and this, in conjunction with the clinical
examination recorded, would not be consistent with his stated inability to
stand for less than 30 minutes. He may need to move around to ease spinal
discomfort but would not need to sit down.”
10 Some customers prefer to stand throughout the interview and this should
be recorded.
Rising and Transferring
11 When considering the ability to rise from sitting to standing, the descriptor
only applies when the customer is unable to rise from sitting without the
assistance of another person. If they could rise using the arms of the chair or
other appropriate aid this descriptor would not apply. The descriptor would be
consistent with severe lower limb problems and muscle wasting. The
functions of the major leg joints have more relevance than lower spinal
function to this activity, since rising can be achieved without spinal flexion.
12 Similarly, the inability to transfer between one seated position and another
indicates significant disability. It reflects those who are wheelchair dependant
and unable to transfer independently. Upper limb function may be relevant in
this activity. For example, a rehabilitated paraplegic who is able to transfer by
use of his upper limbs would not satisfy the transferring descriptor (however
they may well satisfy the higher standing descriptor depending on degree of
lower limb weakness).
Details of activities of daily living
13 The disability analyst considers the customer’s ability in relation to:
• Getting on and off the toilet unaided, without the assistance of another
person.
• The use of public transport in the absence of a companion.
• The use of an adapted car by a wheelchair dependant person.
• Getting in and out of a car; and
• Getting out of chairs or off the bed.Observed behaviour
14 The disability analyst observes the customer’s ability to rise from sitting
and notes the type of chair, when the person is collected from the waiting
area. There is a further opportunity to observe this function during and at the
end of the interview.
Clinical examination
15 Restricted ability to sit and stand will commonly be due to disorders
affecting the lumbar spine or lower limbs. The level of restriction required for
sitting or standing descriptors to apply would indicate that there should be
evidence of positive clinical findings in the majority of cases. Normal
functional ranges of movement for rising are considered. Evidence of muscle
wasting and reduced power in the lower limbs are important clinical findings.
16 Upper limb function is reviewed when considering ability to transfer. A
paraplegic who has suffered a complete spinal cord transaction but who has
good upper limb power may be able to transfer, however a quadriplegic with
an incomplete spinal cord injury who has limited power in both upper and
lower limbs may be unable to transfer.
DLA Considerations
17 The Activity provides information about the ability to stand, to rise from a
chair, to transfer and to sit comfortably. Consideration of the descriptor
chosen will be useful to the DM when determining the help needed with
getting in and out of bed, use of bath/shower, rising from a chair, using the
toilet and preparing a meal.
18 The ability to stand is covered by the two descriptors:-
S (a) Cannot stand for more than 10 minutes, unassisted by another person,
even if free to move around, before needing to sit down.
S (e) Cannot stand for more than 30 minutes, even if free to move around,
before needing to sit down.
19 Musculoskeletal and neurological conditions affecting the lower limbs may
limit the ability to stand. Someone who cannot stand unassisted for more than
10 minutes S (a) is likely to need help with bathing, getting in and out of bed,
the toilet and may need with help with cooking. People who cannot stand for
more than 30 minutes are likely to more independent in respect of these care
needs. Corroboration of a person’s ability to stand will be found in the record
of daily activities e.g. waiting for the bus, queuing at the supermarket check
out, waiting for children outside school.
20 Descriptor S (d) Cannot move between one seated position and
another seated position located next to one another without receiving physical assistance from another person is relevant to a wheelchair user
who cannot transfer unaided.
21 People who require assistance to rise from a chair will be covered in the
report
by descriptor S (c) Cannot rise to standing from sitting in an upright chair
without physical assistance from another person. Note that this refers to
an upright chair without arms. At the medical assessment the disability analyst
will have had the opportunity to observe the person getting up from a chair in
the waiting room and examination room. In the typical day account there may
also be reference to the person’s ability to get in and out of a car, to use the
toilet and the bath.
22 The ability to sit comfortably (descriptors S (b) and S (e)) are of less
relevance to the need for care, and are more applicable to the person’s ability
to perform work related activities.
Bending and kneeling – Activity 3
Descriptors
B (a) Cannot bend to touch knees and straighten up again.
B(b) Cannot bend, kneel or squat, as if to pick a light object, such as a piece
of paper, situated 15cm from the floor on a low shelf, and to move it and
straighten up again without the help of another person.
B(c) Cannot bend, kneel or squat, as if to pick a light object off the floor and
straighten up again without the help of another person.
B (d) None of the above apply
Scope
1 This Activity relates to lower limb and back function. It is intended to reflect
ability to reach a low level such as a low shelf, or the floor, using supports
such as furniture if needed, but without dependence on another person for
support to straighten up again.
2 “As if to pick up an object” does not include the ability to manipulate the
object or the ability to lift weights (these capabilities are covered in other
areas relating to upper limb function).
3 Descriptor B (a) implies a very severe condition, with both lumbar spine and
hip movements severely reduced, or restricted by pain. This activity is very
different from the one involved in descriptors B (b) and B(c). These
descriptors consider the activity of bending and/or kneeling as if to pick
something off the floor or a low shelf which involves a combination of flexing the lumbar spine, flexing the hip joints, and bending the knees to a squatting
position.
Details of activities of daily living
4 The disability analyst considers the customer’s ability in relation to:
• Dressing and undressing especially footwear;
• Getting in and out of the bath;
• Bending to reach the oven, front loading washing machine, low
cupboards or shelves;
• Hanging laundry to dry; and
• Carrying out household cleaning chores.
Bending to tend to babies and toddlers may also be relevant as may leisure
and recreational activities involving bending e.g. gardening, tending to pets.
Observed behaviour
5 The record should obtain observations about general mobility. Functional
knee and hip movement are important for this task and may be observed
while the customer is seated at interview. While it is not appropriate to directly
observe the claimant undressing/dressing the record may note the time taken
and any help requested with certain items of clothing particularly shoes.
6 The disability analyst will observe the customer’s ability to climb on and off
the couch.
7 It may be possible to observe the customer pick up an item such as a
handbag or shopping bag from the floor of the examination room.
Clinical examination
8 Restriction of spinal movement to the degree indicated by B (a) suggests a
severe spinal problem. Clinical examination should be consistent with this.
There may be evidence of muscle wasting. For B (b) or B(c) to apply,
examination would confirm the presence of significant pathology in both knees
and hips. In some neurological conditions an assessment of balance including
tests of cerebellar or proprioceptive function may be recorded. Assessment of
power in the lower limbs is essential.
DLA Considerations
9 Consideration of the descriptor chosen will be useful to the DM in
determining the help needed with dressing, getting in and out of bed, bathing,
rising from chair. The customer whose restriction in bending and kneeling is
described by B (a) or B (b) is likely to need assistance with personal care.10 A person with lumbar back pain who has good hip and knee function would
be expected to be able to bend to an oven safely, since they would not rely
solely on bending their lower back to reach the oven.
Reaching – Activity 4
Descriptors
R (a) Cannot raise either arm as if to put something in the top pocket of a coat
or jacket.
R (b) Cannot put either arm behind back as if to put on a coat or jacket.
R(c) Cannot raise either arm to top of head as if to put on a hat.
R (d) Cannot raise either arm above head height as if to reach for something.
R (e) None of the above apply.
Scope
1 Ability to undertake these activities is determined by shoulder function
and/or elbow function. It is intended to reflect the ability to raise the upper
limbs to a level above waist height.
2This functional category considers the customer’s ability to reach upwards. It
is an evaluation of power, co-ordination, and joint mobility in the upper limbs.
3 All the descriptors apply to people who have functional restriction affecting
both upper limbs i.e. they must have bilateral impairment.
4 It takes into account the ability to achieve the described reaching posture
and does not measure hand function, i.e. it is not necessary for the customer
to adjust the hat if he can achieve the reaching movement defined in
Descriptor R(c) “Cannot raise either arm to top of head as if to put on a hat”.
Details of activity of daily living
5 The disability analyst considers the customer’s ability in relation to:
• Dressing and undressing (including reaching for clothes on shelves/in
wardrobes).
• Hair washing and brushing.
• Shaving.
• Household activities such as reaching up to shelves; putting shopping
away at home; household chores such as dusting; hanging laundry on
a washing line.
• Leisure activities such as aerobics, golf, painting and decorating.Observed behaviour
6 The disability analyst records any spontaneous movements of the upper
limbs, particularly if these are in excess of those elicited by formal
examination.
7 The ease (or otherwise) with which a coat or jacket is removed and
subsequently replaced may be observed. It may be apparent that a stiff or
painful shoulder restricts function.
8 The customer may also hang up a coat or a jacket allowing observation of
spontaneous shoulder and arm action.
Examination
9 The examination shows whether the restriction in reaching is unilateral or
bilateral. If unilateral, the report will state which side is affected and record
normal function in the opposite limb.
DLA considerations
10 Cases in which any of the descriptors R (a) to R (d) have been chosen are
likely to have severe bilateral joint conditions or neurological disorders
affecting function e.g. rheumatoid arthritis, tetraplegia, muscular dystrophy.
This information will be useful to the DM when considering the need for help
with dressing, washing, feeding etc., and will be supported by observations of
upper limb use in the examination centre, and an account of relevant daily
living activities such as ability to dress, wash hair, shave, do household tasks,
drive etc.
11 The Activity does not apply to someone who can reach with one arm only,
whether the dominant arm or not. However if a person has a condition that
affects reaching in one upper limb only, this will be documented in the report.
Clinical findings will be recorded for both the impaired and the normal limb,
and the disability analyst’s opinion in respect of the function in each will be
supported in the usual manner by the observations and the person’s ability to
perform daily tasks. The information is likely to be of value to the DM when
considering the need for help with personal care.
Picking up or moving or transferring objects by use of the upper
body and arms – Activity 5
Descriptors
P (a) Cannot pick up and move a 0.5 litre carton full of liquid with either hand.
P (b) Cannot pick up and move a one-litre carton full of liquid with either hand.P(c) Cannot pick up and move a light but bulky object, such as an empty
cardboard box, requiring the use of both hands together.
P (d) None of the above apply.
Scope
1 This Activity relates mainly to upper limb power, however joint function and
co-ordination of movement are also considered. It is intended to reflect the
ability to pick up and transfer articles at waist level, i.e. at a level that requires
neither bending down and lifting, nor reaching upwards (these capabilities are
covered in other areas). It does not include the ability to carry out any activity
other than picking up and transferring, i.e. it does not include ability to pour
from a carton or jug. Note that the descriptors apply to people who have
functional restriction affecting both upper limbs.
2 All the loads are light and are therefore unlikely to have much impact on
spinal problems. However, consideration is given to neck pain and the
associated problems arising from cervical disc prolapse and marked cervical
spondylitis (arthritis). These conditions may be aggravated by lifting weights in
exceptional circumstances.
3 The ability to carry out these functions is considered with the use of any
prosthesis, aid or appliance.
Details of activities of Daily Living
4 The disability analyst considers the customer’s ability in relation to:
• Cooking (lifting and carrying saucepans, crockery);
• Shopping (lifting goods out of shopping trolley or from the supermarket
shelves);
• Dealing with laundry/carrying the laundry;
• Lifting a pillow;
• Making tea and coffee; and
• Removing a pizza from the oven/ carrying a pizza box.
Observed behaviour
5 The disability analyst observes hand, arm and head gestures. They note the
ease (or otherwise) with which any coat or jacket is removed and replaced.
6 The customer may hang up a coat or a jacket allowing observation of upper
limb function.
7 The customer may lift their handbag or shopping bag several times during
the interview process.8 Where there is a lack of co-operation in carrying out active neck and upper
limb movements then informal observations, coupled with examination of the
upper limbs, may allow an estimate of the usual mobility. This may well be
confirmed by evidence from the typical day.
Examination
9 The report contains information about joint movement and power in the
limbs. Reduced co-ordination or other neurological problems such as tremor
e.g. Parkinson’s disease, is assessed when considering these activities.
DLA Considerations
10 The information in the report will applicable to care needs in respect of
dressing, washing, feeding, preparing a meal etc. The choice of descriptors P
(a) to P(c) is likely to be made in customers who have severe bilateral joint
conditions such as rheumatoid arthritis or neurological disorders such as
multiple sclerosis, Parkinson’s disease.
11 The Activity does not apply to someone who can pick up or transfer with
one arm only, whether the dominant arm or not. However if a person has a
condition that affects one upper limb only e.g. stroke, this will be documented
in the report. Clinical findings will be recorded for both the impaired and the
normal limb, and the disability analyst’s opinion in respect of the function in
each will be supported in the usual manner by the observations and the
person’s ability to perform daily tasks. The information about the impaired limb
is likely to be of value to the DM when evaluating the need for help with
personal care.
Manual Dexterity – Activity 6
Descriptors
M (a) Cannot turn a “star-headed” sink tap with either hand.
M (b) Cannot pick up a £1 coin or equivalent with either hand.
M(c) Cannot turn the pages of a book with either hand.
M (d) Cannot physically use a pen or pencil
M (e) Cannot physically use a conventional keyboard or mouse
M (f) Cannot do up / undo small buttons, such as shirt or blouse buttons.
M (g) Cannot turn a “star-headed” sink tap with one hand but can with the
other.M (h) Cannot pick up a £1 coin or equivalent with one hand but can with the
other
M (i) Cannot pour from an open 0.5 litre carton full of liquid
M (j) None of the above apply
Scope
1 This Activity relates to hand and wrist functions. It is intended to reflect the
level of ability to manipulate objects that a person would need in order to carry
out work-related tasks. Ability to use a pen or pencil is intended to reflect the
ability to use a pen or pencil in order to make a purposeful mark. It does not
reflect a person’s level of literacy. The same concept applies to use of a
computer keyboard/mouse.
2 The efficiency of hand function is considered in relation to the other limb,
i.e., it should not be accepted that one limb can complete a task when this can
only be accomplished with the support of the other limb. For example, the
customer whose right-arm is in a plaster cast where they can only complete
tasks by supporting it with the left arm.
3 “Either” hand in M (a), M (b) or M(c) means they cannot carry out the action
with their right hand and they cannot do it with their left hand.
4 An individual in a forearm plaster may still have good movements of their
hands but the level of pain experienced should be taken into account when
choosing a descriptor, e.g. an individual with a fractured wrist may have good
fine movements of their hand but turning a star headed sink tap would cause
severe pain in their wrist.
Details of Activities of daily living
5 The disability analyst considers the customer’s ability in relation to:
• Filling in forms (e.g. ESA50, national lottery ticket);
• Coping with buttons, zips, and hooks on clothing;
• Cooking (opening jars and bottles; washing and peeling vegetables);
and
• Leisure activities such as reading books and newspapers, doing
crosswords, knitting, manipulating the petrol cap to refuel a car.
Observed behaviour
6 The disability analyst may have the opportunity to observe how the
customer handles tablet bottles, their expenses sheet or a repeat prescription
sheet. They may also be observed lifting objects such as a pen or handling a
newspaper. Fine movements may be seen if the person adjusts their hair, scratches their head or removes spectacles. They may also adjust their watch
or unbutton a shirt cuff for examination.
Examination
7 The disability analyst tests grip and the ability to perform pincer movements
and opposition of the thumb.
8 The report will show whether the problem is unilateral or bilateral. Where the
problem is unilateral, the record will state which side is impaired and comment
on the normal function of the other limb.
DLA Considerations
9 Descriptors M(a), M(b) and M(c) relate to impairment affecting both limbs
and are likely to reflect severe functional limitation in conditions such as
rheumatoid arthritis, multiple sclerosis, motor neurone disease. Information
about manual dexterity is valuable to the DM in respect of dressing, washing,
managing at the toilet, feeding, preparing food. How the person manages
these types of activities on a daily basis will be included in the typical day
account. For example, the ability to prepare a snack or to load a dishwasher
mirrors the tasks undertaken in preparing a meal.
10 Descriptors M (d) to M (i) relate to unilateral impairment only and cover a
much wider range of medical conditions including arthritis, stroke, chronic
regional pain syndrome etc.
Speech – Activity 7
Descriptors
Sp (a) Cannot speak at all
Sp (b) Speech cannot be understood by strangers
Sp(c) Strangers have great difficulty understanding speech
Sp (d) Strangers have some difficulty understanding speech
Sp (e) None of the above apply.
Scope
1 This Activity relates to ability to communicate through speech. It assumes
use of the same language as the person with whom communication is being
attempted. The intention is that it would include impediment to communication
resulting from a severe stammer, but not impediment from speaking with a
local or regional accent. It includes impediment to communication due to expressive dysphasia (inability to express one’s thoughts) resulting from brain
injury.
2 Note that the term “strangers” means persons who do not know the
claimant, but speak in the same language using a similar accent.
3 Speech is an extremely complex activity, involving intellectual, neurological
and musculoskeletal components. It may, therefore, be affected by any
condition involving these areas. In rare cases, it may be that both
psychological and physical factors play a part in the causation of speech
difficulties.
4 Speech problems may occasionally be claimed such that speech is affected
in cases of Chronic Fatigue Syndrome, where the customer asserts that
speech becomes unclear when they are tired. A similar claim may be made by
customers suffering from panic attacks, who describe difficulty in making
themselves understood during an episode of acute anxiety. It may be the case
that such customers should be assessed under the mental function Activities.
The disability analyst considers their ability to make themselves understood
most of the time.
5 Some customers who suffer from breathlessness due to physical causes will
describe difficulty with speech. However, in many of these cases, the problem
is transitory and only occurs during extra physical effort, like walking quickly or
climbing stairs. Therefore, for the majority of the time, they will have normal
speech.
Details of activities of daily living
6 The disability analyst considers the customer’s ability in relation to:
• socialising with family and friends;
• activities such as shopping, or travelling on public transport; and
• use of the telephone.
Observed behaviour
7 The disability analyst describes the quality of speech at interview and any
difficulty they have in understanding the customer. The report will detail any
abnormalities of the mouth and larynx and their effects on speech.
Hearing – Activity 8
Hearing is assessed with a hearing aid or other aid if normally worn
Descriptors
H (a) Cannot hear at allH (b) Cannot hear well enough to be able to hear someone talking in a loud
voice in a quiet room, sufficiently clearly to distinguish the words being spoken
H(c) Cannot hear someone talking in a normal voice in a quiet room,
sufficiently clearly to distinguish the words being spoken
H (d) Cannot hear someone talking in a loud voice in a busy street, sufficiently
clearly to distinguish the words being spoken
H (e) None of the above apply
Scope
1 This Activity relates to the ability to hear speech sufficiently clearly to be
able to follow a conversation. It is intended to take into account hearing aids if
normally worn, but not non-verbal means of communication such as lip
reading or use of sign language.
2 Descriptor H(a) is intended for the person who cannot hear sound even
when maximum volume is used, implying a very severe degree of hearing
loss, which will only apply in exceptional cases e.g. with a binaural hearing
threshold above 90db.
3 A “busy street” does not mean one rendered intolerably noisy by
exceptional machinery such as a juggernaut or earth-moving equipment.
None of us would be able to hold a conversation under such circumstances. It
is however commonplace for pedestrians to talk to each other while busy
traffic passes by. The assessment will consider whether the customer could
hold such a conversation under these circumstances, or whether hearing is so
diminished that background traffic noise would render conversation
impossible.
4 The report will show whether deafness is unilateral or bilateral as stated by
the customer, and how it affects them.
5 The report will describe the person’s ability to wear a hearing aid. If the
person is unable to use the prescribed hearing aid, the report will show the
state the reason why. A customer who has been inconvenienced by a hearing
aid and has abandoned its use should be assessed without aids.
6 It should be remembered that hearing aids can cause distortion of sound
and do not restore ‘normal’ hearing to people with hearing impairments. Older
people may have difficulties adapting to hearing aid use.
7 The report will provide examples of how a person with hearing impairment
communicate in day to day life with family, out shopping, travelling by public
transport etc. People with severe hearing impairment who use British Sign
Language may attend for assessment. In these circumstances the disability
analyst is asked to enquire, via their interpreter, about their ability to communicate when out e.g. by writing a request such where do I catch the
bus to X?
8 For further information on associated problems such as tinnitus, and
Meniere’s disease, see the end of this section.
Details of activities of daily living
9 Significant deafness is such a disadvantage that the customer would be
expected to readily impart details of social isolation and domestic difficulties,
such as problems encountered in communication in shops or on family
occasions, inability to continue particular hobbies e.g. going to the cinema or
theatre, playing bridge or bingo.
10 The report will describe the use of any accessory aids such as
headphones or loop system amplification for TV, radio, or video; amplification
for telephone handset; loud front door bells or door lights.
11 In claimants with profound deafness who communicate through British
Sign Language (BSL), enquiries should have been made via the interpreter
with regard to the standard of BSL that they achieve and how they
communicate in shops, pubs; for example, whether they write a list to hand to
the bar tender.
Observed behaviour
12 The customer’s response to an ordinary or quiet voice during interview is a
good measure of their ability to hear.
13 Very deaf customers often fail to respond to their call in the waiting area;
bring a companion with them to assist them with communication; or function
poorly at the interview requiring the examiner to raise their voice and repeat
questions.
Examination
14 The most relevant examination technique is the conversational voice test.
One ear is masked with the customer’s hand and the customer looks away
from the examiner. The customer is asked to repeat numbers or words or
answer simple questions, which are posed in a normal conversational voice.
The furthest distance away from the ear that the words can be heard is
recorded.
15 The normal ear can detect a conversational voice at 9 metres, which is
impractical in most examination centres. A distance of 3 metres is acceptable
proof of hearing for the purposes of reasonable functional hearing ability.
16 In unilateral hearing loss the normal ear generally compensates for the
deaf one, so the overall hearing loss in such a case is unlikely to be significant. However, checking the hearing in each ear separately and then
both ears together provide opportunity to detect unreliable responses
suggestive of non-organic hearing loss.
Tinnitus
17 Tinnitus the perception of sound where there is no external stimulus. It is
often described as a high-pitched buzzing noise in one or both ears.
18 The use of hearing aids can, by recruitment of background noises, help to
mask tinnitus. Customers may also have developed their own masking
techniques, for example by the use of background music.
Tinnitus maskers may also be prescribed in severe cases.
19 Severe and/or resistant tinnitus can be very disabling and may result in
sleep disturbance, anxiety and depression. The following factors will give
indication of disabling tinnitus:
• Referral to a specialist unit;
• The prescription of maskers/hearing aid;
• The need for night sedation; and
• The prescription of anti-depressant medication.
20 Tinnitus on its own is unlikely to cause functional hearing loss, however it
can significantly impact on concentration. The Mental Function test is carried
out in cases of tinnitus where there is anxiety/depression or other mental
disablement.
Meniere’s disease
21 Meniere’s disease is characterised by recurring bouts of profound,
prostrating vertigo, nausea and vomiting with deafness and tinnitus. Such
attacks can last for anything up to 24 hours, but unsteadiness and loss of
confidence can persist for several further days. Sensorineural low/midfrequency hearing loss and tinnitus may persist between bouts and if the
condition is chronic the deafness may be progressive. The occurrence of
attacks is variable and unpredictable. Management involves symptomatic
treatment of the acute episode and prescription of prophylactic medication.
22 For the purpose of the LCW/LCWRA, the disability analyst records the
frequency and duration of the attacks, and also the therapeutic measures
being taken to control the condition, and the effectiveness of the measures.
23 The effects of the Meniere’s disease should be fully taken into account
when choosing physical descriptors (i.e. the activity must be performed safely,
reliably and repeatedly).DLA Considerations
24 People with significant degrees of hearing loss represented by descriptors
H(a) to H(c) will be assessed at the WCA with a view to facilitating a return to
work, or entry into work for those who have not worked previously e.g. people
with congenital deafness. The report will provide information on how they
communicate on a day to day to basis including use of BSL, and whether they
have any additional learning disabilities or mental health problems that might
increase their level of disability. The information will be of use to the DM both
in determining care needs and their ability to get around on their own
Vision – Activity 9
Vision including visual acuity and visual fields, in normal daylight or bright
electric light, with glasses or other aid to vision if such aid is normally worn
Descriptors
V (a) Cannot see at all
V (b) Cannot see well enough to read 16 point print at a distance of greater
than 20cm
V(c) Has 50% or greater reduction of visual fields
V (d) Cannot see well enough to recognise a friend at a distance of at least 5
metres
V (e) Has 25% or more but less than 50% reduction of visual fields
V (f) Cannot see well enough to recognise a friend at a distance of at least 15
metres
V (g) None of the above apply
Scope
1 The Activity is vision in normal daylight or bright electric light, with glasses
or other visual aids, which would normally be worn. It relates to visual acuity
(central vision and focus) and to visual fields (peripheral vision). It is intended
to reflect the activity of seeing clearly without taking literacy into account.
2 16-point print is intended to reflect central vision, and should be enough to
allow a person to read a reasonable amount of text at a time, not just
individual letters. However it does not include ability to sustain concentration
while reading or literacy.
3 “Recognising a friend” implies the ability to recognise a friend’s features, not
to recognise them, for example, from the clothes they are wearing.4 Normal vision is taken as visual acuity of 6/6 at a distance of 6 metres from
the Snellen chart. To hold a class 1 driving licence (permits driving of a private
car) in the UK, acuity of 6/10 on the Snellen chart is required.
5 Vision has to be useful vision in the context of a normal environment. A
condition causing severe tunnel vision where, despite reasonable visual
acuity, an individual cannot read whole sentences or scan a page, causes
significant disability. An appropriate descriptor in this situation would be V(b)
6 Visual field loss is considered in the LCW/LCWRA. Visual field loss may
result in significant functional limitations and can be caused by a number of
conditions such as glaucoma, retinopathy or homonymous hemianopia. It may
reduce safety awareness in situations such as traffic or cause a tendency to
falls.
Details of Activities of daily living
7 The disability analyst considers the customer’s ability in relation to:
• Filling in forms;
• Driving – both from the visual acuity and visual field point of view;
• History of falls or accidents;
• Use of public transport – getting on and off buses unassisted, reading
the bus name and number;
• Mobilising independently outdoors;
• Reading newspapers or magazines, watching television;
• Helping children with homework or reading bedtime stories; and
• Leisure activities, in particular participatory sports such as snooker or
darts and activities that require good vision such as knitting or sewing.
Observed behaviour
8 The disability analyst records how the customer got to the examination
centre, and how they found their way around the centre, and whether they
needed to be accompanied by another person.
9 The disability analyst observes their actions when navigating obstacles, for
example, do they rotate their neck more to adjust for reduced visual fields?
10 They will also observe their ability to manipulate belts and buttons, and
whether the claimant is able to read their medication labels or repeat
prescription sheet.
Examination
11 The report includes the aided binocular vision, and explains its significance
to the Decision Maker.12 If the customer forgets their spectacles but there is evidence from the
typical day activities and behaviour observed that there is no significant
disability with vision, then this will be reflected in the descriptor choice. In
these cases or in cases where the VA is poor but the examiner thinks that it
could improve with correction, it can be measured it using a pinhole, (in effect
this replaces a spectacle lens as in a pin hole camera).
13 Near vision is recorded using a near vision chart. N8 print is the equivalent
of normal newsprint.
14 Where there is a history of any visual field problem or where the analyst at
assessment thinks that there may be a visual field problem, visual fields are
tested by clinical examination.
15 For the purposes of the LCW/LCWRA, the examiner will provide an opinion
of visual field loss of 50% or greater (descriptor Vc) or loss of 25% or more
but less than 50 % (descriptor Ve) than normal.
DLA considerations
16 For people with visual impairment the report contains a record of their
visual acuities. In addition it will also contain information about any reduction
in visual fields. The latter is expressed as a percentage reduction.
17 A person should be able to dress themselves if vision meets the descriptor
V(b) or better i.e. V(b) Cannot see well enough to read 16 point print at a
distance of greater than 20cm.
18 A person should be able to find their way around if their vision is V (f) or
better i.e. – Cannot see well enough to recognise a friend at a distance of
at least 15 metre.
19 The disability analyst will have observed the ease with which the customer
moves around the examination centre, their ability to read documentation, to
manage personal possessions such as a handbag and to make eye contact
during interaction. Their ability to watch TV, go shopping, to drive and partake
in leisure activities will have been explored in the typical day interview.
Continence – Activity 10
This Activity is subdivided under 3 sets of descriptors – 10(a), 10(b), and 10(c)
Activity 10 (a) Continence other than enuresis (bed-wetting) where the
person does not have an artificial stoma or urinary collecting device.
Descriptors
C (a) Has no voluntary control of the evacuation of the bowelC (b) Has no voluntary control of the voiding of the bladder.
C(c) At least once a month loses control of bowels so that the person cannot
control the full evacuation of the bowel.
C (d) At least once a week loses control of bladder so that the person cannot
control the full voiding of the bladder.
C (e) Occasionally loses control of bowels so that the person cannot control
the full evacuation of the bowel.
C (f) At least once a month loses control of bladder so that the person cannot
control the full voiding of the bladder.
C (g) Risks losing control of bowels or bladder so that the person cannot
control the full evacuation of the bowel or the full voiding of the bladder if not
able to reach a toilet quickly
C (h) None of the above apply
Scope
1 This functional area describes total involuntary voiding of bowel or bladder,
not just minor leakage as might occur with minor degrees of stress
incontinence.
2 The descriptors cover an assessment of continence while the customer is
awake. Incontinence which occurs only while asleep (enuresis) is not
regarded as incontinence in terms of the legislation as, with the appropriate
personal hygiene, this will not affect the person’s functioning whilst awake e.g.
at work.
3 Similarly, incontinence occurring during a seizure happens during a period
when there is a period of altered consciousness, so incontinence will not of
itself affect functioning. Seizures should be considered under the appropriate
functional area.
4 Urgency, as typically associated with prostatism, will not usually meet the
criteria for `incontinence’ or `loss of control’, as it can be controlled by regular
voiding. Customers with gastro-intestinal problems or frequency of micturition
should be considered as possibly meeting the criteria for C (g), when their
problem is unpredictable to the extent that they would become incontinent, if
they did not leave their work place immediately or within a very short space of
time.
5 In situations where a customer has problems of control with both the
bladder and the bowels the highest descriptor should be applied, e.g. in a
customer who loses control of bladder function at least once a month (C (f))
and who also loses control of their bowels occasionally (C (e)) the higher of
the two descriptors (C (e)) should be chosen. 6 `Occasionally’ implies less than once a month or, happening irregularly with
an overall frequency of less than once a month.
7 ‘No voluntary control’ – means that the person is unable to determine, by
conscious effort, when the bladder or bowels discharge.
8 Mild stress related incontinence, where the person has voluntary control
over the bladder for most of the time but such control is lost at certain times,
would not amount to ‘no voluntary control over the bladder’.
Details of activities of daily living
9 The disability analyst considers the customer’s ability in relation to:
• the frequency and length of any journeys or outings undertaken, e.g.
shopping trips, car journeys ;
• Visits to friends or relatives;
• Other social outings;
and any problems encountered in undertaking these activities. The clinical
diagnosis, medication and previous investigations or specialist input are taken
into account.
Activity 10 (b) Continence where client uses a urinary collecting device,
worn for the majority of the time including an indwelling urethral or
suprapubic catheter.
Descriptors
CU (a) Is unable to affix, remove or empty the catheter bag or other collecting
device without receiving physical assistance from another person
CU (b) Is unable to affix, remove or empty the catheter bag or other collecting
device without causing leakage of contents.
CU(c) Has no voluntary control over the evacuation of the bowel
CU (d) At least once a month loses control of bowels so that the person
cannot control the full evacuation of the bowel.
CU (e) Occasionally loses control of the bowel so that the person cannot
control the full evacuation of the bowel.
CU (f) Risks losing control of bowels so that the person cannot control the full
evacuation of the bowel if not able to reach a toilet quickly
CU (g) None of the above applyScope
10 This functional category reflects the ability of an individual to manage their
urinary continence by use of a urinary collecting device. It should be noted
that for the purposes of the legislation, a urostomy is considered as a urinary
collecting device.
11 Therefore, a person who has no bowel continence issues and can
successfully manage to maintain their urinary collecting device without
spillage, would not score in this category.
12 In this area, a stoma that is poorly functioning, or has a fistula or is poorly
fashioned such that leakage is a common occurrence should be considered
as CU (b).
13 Upper limb function and mental abilities must be considered in this activity
in relation to the person’s ability to cope with the collecting device.
Activity 10(c) Continence other than enuresis (bed wetting) where the
person has an artificial stoma.
Descriptors
CB (a) Is unable to affix, remove or empty stoma appliance without receiving
physical assistance from another person.
CB (b) Is unable to affix, remove or empty stoma appliance without causing
leakage of contents.
CB(c) Where the person’s artificial stoma relates solely to the evacuation of
the bowel, at least once a week, loses control of bladder so that the person
cannot control the full voiding of the bladder.
CB (d) Where the person’s artificial stoma relates solely to the evacuation of
the bowel, at least once a month, loses control of bladder so that the person
cannot control the full voiding of the bladder.
CB(e) Where the person’s artificial stoma relates solely to the evacuation of
the bowel, risks losing control of the bladder so that the person cannot control
the full voiding of the bladder if not able to reach a toilet quickly.
CB (f) None of the above apply
Scope
14 This functional category reflects the ability of an individual to manage their
artificial stoma.15 Therefore, a person who has no problem with urinary continence and can
successfully manage to maintain their stoma without leakage would not score
in this category.
16 In this area a stoma that is poorly functioning, or has a fistula or is poorly
fashioned such that leakage is a common occurrence should be considered
as CB (b).
17 Upper limb function and mental abilities must be considered in this activity
in relation to the person’s ability to cope with the artificial stoma.
DLA Considerations
18 Activity 10(a) relates to urinary and/or bowel continence where the person
does not have a stoma or urinary collecting device. It reflects the amount of
voluntary control that the person has over micturition or defaecation, and how
often incontinence occurs. The report provided useful information regarding
the diagnosis of the underlying medical condition causing the incontinence,
any special investigations undertaken and medication taken.
19 Activity 10(b) applies to people who wear for the majority of the time a
urinary collecting device such as a urinary catheter, urethral sheath,
suprapubic catheter or urostomy. It provides information as to whether the
person needs physical assistance from another person to manage the
catheter bag or who cannot manage the bag without causing leakage. This
could be because the person lacks manual dexterity e.g. rheumatoid arthritis,
or because they have learning disabilities.
20 Activity 10 (c) applies to people who have artificial stomas. It identifies
people who need physical assistance from another person to manage the
stoma bag, or who cannot mange the bag without causing leakage.
21 Although information in the Continence section of the report appears
complex, it will be very helpful to the DLA DM in identifying individuals who
have medical conditions causing urinary and/or bowel incontinence of a
substantial nature, and in recording how often the incontinence occurs. For
people who have artificial stomas or long-term urinary catheters (or other
urinary collecting devices), the report contains information on those who need
help from others to manage on a day-to-day basis.
Remaining conscious during waking moments – Activity 11
Descriptors
F (a) At least once a week, has an involuntary episode of lost or altered
consciousness, resulting in significantly disrupted awareness or
concentration.F (b) At least once a month has an involuntary episode of lost or altered
consciousness, resulting in significantly disrupted awareness or
concentration.
F(c) At least twice in the six months immediately preceding the assessment,
has an involuntary episode of lost or altered consciousness, resulting in
significantly disrupted awareness or concentration
F (d) None of the above apply
Scope
1 This Activity covers any involuntary loss or alteration of consciousness
resulting in significantly disrupted awareness or concentration occurring
during the hours when the customer is normally awake, and which prevents
the customer from safely continuing what they are doing. Such events
occurring when the customer is normally asleep are not taken into
consideration. The descriptors relate to the frequency with which such
episodes of lost or altered consciousness occur. It should be noted that the
descriptor indicates that awareness must be significantly disrupted. This
means the nature of the episodes and their effects on function must be
explored to see if they fulfil the criteria.
2 In the context of WCA, the most likely causes of episodes of “lost
consciousness” are:
• Generalised seizures (previously referred to as grand mal, tonic clonic
and myoclonic seizures).
• A seizure which is secondary to impairment of cerebral circulation.
• Cardiac arrhythmia.
• “Altered consciousness” implies that, although the person is not fully
unconscious, there is a definite clouding of mental faculties resulting in
loss of control of thoughts and actions. The causes most likely to be
encountered are:
i. Partial seizures which may simple or complex partial (previously
known temporal lobe epilepsy); or
ii. Absence seizures which may be typical (petit mal) or atypical; or
iii. Hypoglycaemia.
For both lost and altered consciousness, establishing an exact diagnosis is
less important than establishing whether or not any disability is present.
3 Any functional limitations due to side effects of medication taken to control
seizures are taken into account. A mental function assessment should be
performed if the side effects of medication are sufficient to interfere with
cognitive ability or produce other mental disablement.4 Giddiness, dizziness, and vertigo, in the absence of an epileptic or similar
seizure, do not amount to a state of “altered consciousness”. These
conditions are therefore not taken into account when assessing the functional
area of remaining conscious. If they affect functional ability in other
categories, they should be taken into account when considering the relevant
Activities.
5 The disability analyst considers whether a customer’s claimed frequency of
seizures is medically reasonable. For example, if there is no corroborative
evidence from the GP and the person is not on any appropriate medication,
this would raise doubts as to a claim of frequent episodes of lost or altered
consciousness.
Details of activities of daily living
6 The disability analyst considers the customer’s ability in relation to:
• driving – the DVLA does not issue a licence to anyone who has had a
daytime seizure in the past year.
• potentially hazardous domestic activities such as cooking.
• recreational activities e.g. swimming, contact sports.
DLA considerations
7 This section of the report relates to people with epilepsy including grand mal
seizures, temporal lobe epilepsy and absence seizures such as petit mal. It
also includes alterations in consciousness due to cardiac arrhythmias and
hypoglycaemia. It does not include giddiness, dizziness, and vertigo.
8 The frequency of the episodes of lost or altered consciousness determines
the descriptor that is chosen. The disability analyst takes into account the
diagnosis, hospital investigations and medication prescribed when evaluating
this Activity. If there is no corroborative evidence of the medical condition from
the general practitioner and the customer is not on any appropriate
medication, it is unlikely that functional limitation due to lost or altered
consciousness will be credited.
9 Information in this section of the ESA 85 is useful to the DM in establishing
the diagnosis, investigation and treatment of the medical condition affecting
consciousness, and the frequency of episodes. It is less helpful in establishing
whether the person has useful warning of the episode, if preventative
measures could be taken and the amount of supervision that the person might
require.
Section 13 – Summary of ESA 85 physical
function information for DLACare needs Functional
Activity
groups
Main ESA
Activity
to consider
Notes Other
Activities to
consider
Getting in
and out of
bed
Lower limbs,
lumbar spine,
upper limbs
Standing &
sitting,
Bending or
kneeling
Walking,
Picking up and
transferring
(ability to push
up)
Getting up
from chair
Lower limbs,
lumbar spine,
upper limbs
Standing &
sitting
Refers to an
upright chair
with no arms.
Includes
wheelchair
transfer
Walking,
Bending or
Kneeling
Washing,
Bathing/use
of shower
Lower limbs,
lumbar spine,
upper limbs
Standing &
sitting
Walking,
Bending or
Kneeling,
Picking up and
transferring
Dressing Upper limbs,
Vision
Manual
dexterity,
Vision
Should be able
to dress if
vision is Vb or
better
Reaching,
Bending or
Kneeling
Feeding Upper limbs Manual
dexterity
Reaching,
Vision
Preparing a
meal
Upper limbs
Cognition
Manual
dexterity
Mental
function
Picking up and
transferring,
Vision
Continence Urinary and
bowel (not
nocturnal
enuresis)
Continence Includes ability
to manage
catheters and
artificial
stomas
Manual
dexterity,
Vision, Mental
Function
Walking
(Mobility)
Lower limbs Walking With aids if
used. Includes
stairs
Getting
around
Vision,
Hearing,
Mental
function
Vision,
Mental
Function
Should be able
to find way
around if vision
is Vf or betterSection 14 – The Mental Function Assessment
and its use in DLA
In this section detailed information about each of the Mental Function
Activities and the ranked descriptors is provided. An explanation of the scope
of each Activity is combined with notes about the type of specific evidence
that the disability analyst takes into account in making their descriptor choice.
For each Activity additional guidance on how the ESA 85 report may be used
to evaluate attention, supervision and getting around (DLA considerations) is
provided.
Note that the Mental Function Activities are grouped together:-
Understanding and focus (Activities 12, 13, 14, 15 and 16)
• Learning or comprehension in the completion of tasks;
• Awareness of hazard;
• Memory and concentration;
• Execution of tasks; and
• Initiating and sustaining personal action.
Adapting to change (Activities 17, 18 and 19)
• Coping with change;
• Getting about; and
• Coping with social situations.
Social Interaction (Activities 20 and 21)
• Propriety of behaviour with other people; and
• Dealing with other people.
Learning or comprehension in the completion of tasks – Activity
12
Descriptors
LT (a) Cannot learn or understand how to successfully complete a simple
task, such as setting an alarm clock, at all.
LT (b) Needs to witness a demonstration, given more than once on the same
occasion of how to carry out a simple task before the person is able to learn
or understand how to complete the task successfully, but would be unable to
successfully complete the task the following day without receiving a further
demonstration of how to complete it.LT(c) Needs to witness a demonstration of how to carry out a simple task,
before the person is able to learn or understand how to complete the task
successfully, but would be unable to successfully complete the task the
following day without receiving a verbal prompt from another person.
LT (d) Needs to witness a demonstration of how to carry out a moderately
complex task, such as the steps involved in operating a washing machine to
correctly clean clothes, before the person is able to learn or understand how
to complete the task successfully, but would be unable to successfully
complete the task the following day without receiving a verbal prompt from
another person.
LT (e) Needs verbal instructions as to how to carry out a simple task before
the person is able to learn or understand how to complete the task
successfully, but would be unable, within a period of less than one week, to
successfully complete the task without receiving a verbal prompt from another
person.
LT (f) None of the above apply.
Scope
1 This Activity reflects ability to learn and understand information. “Learning”
assesses the ability to learn and retain information; while “understanding” is
about comprehension of information. This activity is intended to be relevant to
learning disability of whatever cause, including the result of acquired brain
injury. It also reflects difficulties in understanding language, such as receptive
dysphasia.
2 It should be noted that some of the descriptors refer to a demonstration
rather than a prompt. This reflects a higher level of disability in that the person
would be unable to remember how to do the task. For example in LT(b), the
person would need to be shown how to push the buttons on the alarm clock,
but in LT(d), being reminded how to do the task would suffice – i.e. they would
not need to be shown physically how to push the button.
3 A simple task may only involve one or two steps while a moderately
complex task may involve 3 or 4 steps.
Details of activities of daily living
4 The disability analyst considers basic functions of personal care such as
brushing teeth. This would involve remembering to put toothpaste onto a
brush and brushing all areas of teeth. This may be regarded as a simple task.
Other aspects of personal care may be the ability to be able to get up,
showered, shave, clean teeth, select clothing items and get dressed
appropriately for the weather outside. This may represent an ability to
understand and retain information.5 Other leisure activities that may be considered include using a TV remote
control, using a stereo by loading the CD into the CD player and selecting the
appropriate function on the stereo to allow the CD to play. Ability to use a Play
station or computer might be relevant in this functional category.
6 Ability to drive, previous employment or tasks learned in training may also
be relevant.
Mental State Examination
7 Clinical findings include record of memory and concentration, general
decision-making ability at assessment, ability to cope at interview, general
intelligence, requirement for prompting etc. The disability analyst may
undertake specific tests of memory and concentration.
DLA Considerations
8 This Activity is intended to be relevant to people with learning disabilities,
brain injury and dementia. The highest level descriptors LT (a) & LT (b) will be
applied to those with the most severe learning disabilities, and the DM should
consider the need for prompting in respect of self-care, and also the
requirement for supervision in some cases. The lower level descriptors LT (c),
LT (d) and LT (e) are also likely to be applicable to people who need
prompting and help with main meal preparation.
Awareness of hazards – Activity 13
Descriptors
AH (a) Reduced awareness of the risks of everyday hazards (such as boiling
water or sharp objects) would lead to daily instances of or to near-avoidance
of:
(i) injury to self or others; or
(ii) significant damage to property or possessions,to such an extent that
overall day to day life cannot successfully be managed.
AH (b) Reduced awareness of the risks of everyday hazards would lead for
the majority of the time to instances of or to near-avoidance of:
(i) injury to self or others; or
(ii) significant damage to property or possessions, to such an extent
that overall day to day life cannot successfully be managed without
supervision from another person.
AH (c) Reduced awareness of the risks of everyday hazards has led or would
lead to frequent instances of or to near-avoidance of:(i) injury to self or others; or
(ii) significant damage to property or possessions, but not to such an
extent that overall day to day life cannot be managed when such
incidents occur.
AH (d) None of the above apply
Scope
1 This Activity is intended to reflect risks from common hazards that may be
encountered by people with reduced awareness of danger through learning
difficulties, or conditions affecting concentration, including detrimental effects
of medication; or from brain injury or other neurological conditions affecting
self-awareness.
2 The Activity reflects a lack of understanding that something is dangerous or
that there is an impaired recognition that a situation will present a potential
hazard. For example a person with dementia may lack insight with regard to
the reason it may be dangerous for them to cook – they lack the ability to
recognise that they are at risk of forgetting that the cooker is on.
Details of activities of daily living
3 When considering this functional category the disability analyst will ask
about ability to cope with potential hazards, and whether the person could be
safely left alone to manage basic daily life. Potential scenarios include:
• Ability to cope with road safety awareness;
• Driving;
• Ability in the kitchen;
• Awareness of electrical safety; and
• Responsibility for children/pets.
Mental State Examination
4 Cognitive issues are important in assessing this functional activity.
5 Insight will also be an important factor and consideration will be given as to
whether the customer has adequate insight into their problems to recognise
the risks present, and therefore whether they are able to avoid potentially
hazardous situations.
DLA Considerations
6 Descriptors AH (a) and AH (b) would be relevant to a need for supervision in
customers with learning disabilities, brain injury etc., and also may be helpful
in considering whether they need guidance when getting around out of doors.
It is not envisaged that the descriptors apply to people with suicidal intent who have clear mental faculties and understand the implications of such an
attempt.
Memory and concentration – Activity 14
Descriptors
7 MC (a) On a daily basis, forgets or loses concentration to such an extent
that overall day to day life cannot be successfully managed without receiving
verbal prompting, given by someone else in the person’s presence.
MC (b) For the majority of the time, forgets or loses concentration to such an
extent that overall day to day life cannot be successfully managed without
receiving verbal prompting, given by someone else in the person’s presence
MC(c) Frequently forgets or loses concentration to such an extent that overall
day to day life can only be successfully managed with pre-planning, such as
making a daily written list of all tasks forming part of daily life that are to be
completed
MC (d) None of the above apply
Scope
1 This activity is intended to be relevant to lapses in memory or concentration
due to fatigue, anxiety, depression, delusions, hallucinations, memory loss,
brain injury or dementia. It also reflects difficulties with memory or
concentration that result from detrimental effects of medication, such as
drowsiness or sedation.
2 It should be noted that in MC (a) and MC (b) that the prompting must be
given in the presence of another person. Prompting via telephone would not
reflect the severity of disability in MC (a) or MC (b). These descriptors reflect a
very severe level of functional restriction.
3 In MC(c) the lists do not reflect the type of lists that could reasonably be
expected to be utilised by those with normal cognitive function such as
shopping lists. The descriptor reflects a need to have additional input to
manage all tasks involved in daily life such as remembering to get washed
and dressed.
Details of activities of daily living
4 When considering this activity, the customer’s ability to live alone or attend
appointments alone should be considered. It would seem unlikely that those
who live alone without substantial input from a carer would have the level of
disability reflected in these descriptors.
5 Abilities that are considered by the disability analyst include:• Attending to personal care;
• Coping with medication;
• Significant accidents at home;
• Shopping;
• Reading/TV;
• Driving;
• Attending to nutrition; and
• Dealing with finances and bills.
Mental State Examination
6 On examination, it would be expected that a severe level of cognitive
impairment would be evident for any of the above descriptors to apply. Mild
impairment of concentration or memory would not normally be consistent with
the level of disability reflected in the descriptors MC (a), MC (b) or MC(c).
DLA Considerations
7 Descriptors MC (a), MC (b) and MH (c) will applicable to people with
learning disabilities, brain injury and dementia. Only those with the most
severe levels of functional restriction due to depression, schizophrenia and
generalised anxiety disorder requiring long-term medication and care from the
mental health team are likely to be covered by these descriptors.
Consideration should be given to the need for prompting or supervision.
Execution of tasks – Activity 15
Descriptors
ET (a) Is unable to successfully complete any everyday task.
ET (b) Takes more than twice the length of time it would take a person without
any form of mental disablement, to successfully complete an everyday task
with which the claimant is familiar.
ET(c) Takes more than one and a half times but no more than twice the length
of time it would take a person without any form of mental disablement to
successfully complete an everyday task with which the claimant is familiar.
ET(d) Takes one and a half times the length of time it would take a person
without any form of mental disablement to successfully complete an everyday
task with which the claimant is familiar.
ET (e) None of the above apply.
Scope
1 This Activity reflects the ability to carry out a task within a reasonable time. It
is intended to reflect difficulties that may be encountered by people with obsessive-compulsive disorder (OCD), learning disability or brain injury. It
includes the effect on a person of experiencing a panic attack – a specific and
overwhelming experience of fear, precluding any form of normal activity. It is
also intended to reflect the impact on carrying out a task that hallucinations or
delusions may have on individuals with psychotic or dissociative states. It may
be compounded by the effects of medication.
2 The descriptors reflect an increased time to complete a task, not a lack of
motivation to commence a task. For example a person with severe OCD may
take several hours to manage to get washed and dressed due to hand
washing rituals preventing them from continuing a task.
3 It should also be noted that this Activity relates to mental disablement and
not physical disablement. For example, a person with rheumatoid disease
with no form of mental disablement, who has significant morning stiffness and
takes several hours to get washed and dressed due to their joint problems,
would not be included in this Activity.
Details of activities of daily living
4 The disability analyst considers routine activities and what would be
reasonable for a person taking into account normal variation in a population
without any form of mental disablement. For example, one person getting up
in the morning may only take 20 – 30 minutes to be up, showered and dressed
to leave for work, but others may take longer – perhaps an hour or slightly
more. It may be useful to consider the overall typical day function. In this
descriptor, further enquiry and clarification of detail will be necessary. For
example, a customer may indicate that they rise at 8.30am but do not get
dressed to get out to shopping until midday. This may initially seem an
excessive time for this activity, however on further questioning it may be
apparent that they choose to watch morning television after their shower and
complete housework before dressing.
5 It must also be considered whether time taken to complete a task is due to
personal preference or choice rather than mental disablement. For example a
person with joint disease or back pain may choose to lie in a bath for an hour
to help alleviate stiffness or simply because they enjoy relaxing in the bath.
6 The pattern of typical day activity should reflect a person who would
struggle to get through the basics of a day due to their mental disablement as
a result of tasks taking so long to complete, that they would be unable to cope
with work. For example those who have severe and continuous disabling
anxiety, where they struggle to even get out of their bedroom, may come into
this category.
Mental State Examination
7 Assessment of cognition, evidence of abnormal perceptions and behaviour
are required in the report. Those with anxiety or depression would be
expected to have Mental State Examination findings consistent with severe levels of anxiety where they may be extremely distracted, distressed or
sweating. In those with significant depression, there may be evidence of slow
speech or slow movements (psychomotor retardation).
DLA considerations
8 People with the most severe levels of anxiety, severe depression i.e. with
psychomotor retardation, severe OCD, schizophrenia, learning disabilities &
brain injury are likely to be restricted in their ability to execute tasks. Those
whose level of restriction is described by ET (a) to ET (d) may need help with
self-care or main meal preparation.
Initiating and sustaining personal action – Activity 16
Descriptors
IA (a) Cannot, due to cognitive impairment or due to a severe disorder of
mood or behaviour, initiate or sustain any personal action (which means
planning, organisation, problem solving, prioritising or switching tasks).
IA (b) Cannot, due to cognitive impairment or due to a severe disorder of
mood or behaviour, initiate or sustain personal action without requiring daily
verbal prompting given by another person in the person’s presence.
IA(c) Cannot, due to cognitive impairment or due to a severe disorder of mood
or behaviour, initiate or sustain personal action without requiring verbal
prompting given by another person in the person’s presence for the majority
of the time.
IA(d) Cannot, due to cognitive impairment or due to a severe disorder of mood
or behaviour, initiate or sustain personal action without requiring frequent
verbal prompting given by another person in the person’ presence.
IA (e) None of the above apply
Scope
1 This Activity reflects the ability to initiate or sustain action without need for
external prompting. It is intended to reflect difficulties that may be
encountered by people with conditions such as depressive illness that result
in apathy, or abnormal levels of fatigue, or abnormal levels of anxiety. It is
also common in some people with schizophrenia. It may be compounded by
the effects of medication.
2 The intention of the activity is to assess whether a person has the capability
to carry out routine day-to-day activities or activities that may normally be
associated with work.
3 “Personal action” may include:• ability to plan and organise a simple meal;
• ability to get up, washed, dressed and ready for work in the morning;
and
• ability to cope with simple household tasks e.g. sorting laundry and
using a washing machine.
Details of activities of daily living
4 Areas considered by the disability analyst will include any behaviour that
involves a decision to plan or organise a personal action to enable the
customer to perform it. Activities may include:
• Making travel arrangements;
• Writing shopping lists;
• Organising finances;
• Planning a simple meal;
• Getting washed and dressed;
• Ironing clothes for the next day; and
• Caring for children, preparing clothing, lunches etc.
Mental State Examination
5 General memory, concentration, intelligence and severity of depression
should be recorded. It should be noted that the descriptors refer to a severe
disorder of mood.
DLA Considerations
6 Descriptors IA (a), IA (b) And IB (c) are relevant to customers with
depression, severe anxiety, schizophrenia etc. who are at danger of selfneglect without prompting. Help with main meal preparation might be
appropriate in someone covered by descriptor IA (d).
Coping with change – Activity 17
Descriptors
CC (a) Cannot cope with very minor, expected changes in routine, to the
extent that overall day to day life cannot be managed.
CC (b) Cannot cope with expected changes in routine (such as a prearranged permanent change to the routine time scheduled for a lunch break),
to the extent that overall day to day life is made significantly more difficult.
CC(c) Cannot cope with minor, unforeseen changes in routine (such as an
unexpected change of the timing of an appointment on the day it is due to
occur), to the extent that overall, day to day life is made significantly more
difficult.CC (d) None of the above apply
Scope
1 This Activity relates to the flexibility needed to cope with changes in normal
routine. It is intended to reflect difficulties that may be encountered by people
with severe learning disability, autistic spectrum disorder, brain injury or
psychotic illness. It is not intended to reflect simple dislike of changes to
routine, but rather the inability to cope with them.
2 It reflects a significant level of functional restriction where small changes
result in the individual’s day to day life being significantly affected i.e. day to
day life is made significantly more difficult or cannot be managed.
Activities of daily living
3 In this functional activity the disability analyst will consider the person’s
ability to cope in situations where some change is possible. Areas to consider
may include:
• Use of public transport;
• Shopping;
• Dealing with appointments at hospital, GP or Jobcentre Plus;
• Coping with children and their out of school activities; and
• Dealing with telephone calls.
4 It may be useful to consider some of these activities in terms of the level of
disability intended, for example:
• A customer who becomes so upset by the phone ringing that they
cannot function beyond that, rather than just feeling stressed or
anxious.
• A customer with a severe form of mental disablement who may
become so distressed by the supermarket being out of stock of their
usual brand of breakfast cereal that they cannot continue with other
activities or complete the rest of their shopping.
• A customer who would be unable to cope with the train being cancelled
and would return home rather than wait for the next train.
Mental State Examination
5 Customers may have poor rapport and be extremely anxious at interview. It
may be that they have been unable at all to attend the MEC for assessment. It
would seem unlikely that a customer who manages to attend the MEC alone
would meet the level of severity of functional restriction for anything other than
CC (d) to apply.DLA Considerations
6 The descriptors are intended to apply to people with functional restrictions
due to severe learning disability, autistic spectrum disorder, brain injury or
psychotic illness e.g. schizophrenia.
7 This Activity is more relevant to difficulties that people with these medical
conditions might have in coping with work or in the work place or in travelling
to work. It is probably of less help to the DM than some other Activities in
determining need for prompting, supervision or getting around.
Getting about – Activity 18
Descriptors
GA (a) Cannot get to any specified place with which the person is, or would
be, familiar.
GA (b) Is unable to get to a specified place with which the person is familiar,
without being accompanied by another person on each occasion.
GA(c) For the majority of the time is unable to get to a specified place with
which the person is familiar without being accompanied by another person.
GA (d) Is frequently unable to get to a specified place with which the person is
familiar without being accompanied by another person.
GA (e) None of the above apply
Scope
1 This Activity relates to an inability to travel without support from another
person, as a result of disorientation; or of agoraphobia causing fear of
travelling unaccompanied. It does not reflect lesser degrees of anxiety about
going out, nor does it reflect planning and timekeeping.
Activities of daily living
2 The disability analyst considers how the person functions taking into
account their level of anxiety and ability to leave the house. Activities include:
• Shopping;
• Attending the pharmacy;
• Attending hospital or GP appointments;
• Walking the dog;
• Supervising children outdoors; and
• General safety awareness and abilities in kitchen may support
significant cognitive disruption resulting in safety issues if going out
unaccompanied.Mental State Examination
3 Intelligence and cognitive function are assessed. It would be expected that
evidence of severe anxiety would be found on examination to support the
level of functional restriction. Lesser degrees of anxiety would not fulfil the
criteria. The descriptors reflect the effects of true panic disorder or severe
agoraphobia.
DLA Considerations
4 The descriptors reflect the difficulties that people with learning disabilities,
brain injury, and dementia experience in getting around due to cognitive
impairment. They also apply to individuals with severe panic disorder and
agoraphobia. Consideration of this Activity will be of use to the DM in
determining whether people with these medical conditions require guidance
and/or supervision out of doors.
Coping with social situations – Activity 19
Descriptors
CS (a) Normal activities, for example, visiting new places or engaging in
social contact, are precluded because of overwhelming fear or anxiety.
CS (b) Normal activities, for example, visiting new places or engaging in
social contact, are precluded for the majority of the time due to overwhelming
fear or anxiety.
CS(c) Normal activities, for example, visiting new places or engaging in social
contact, are frequently precluded, due to overwhelming fear or anxiety.
CS (d) None of the above apply.
Scope
1 This Activity is intended to reflect lack of self-confidence in social situations,
which is greater in its nature and its functional effects than mere shyness or
reticence. It reflects levels of anxiety that are much more severe than fleeting
moments of anxiety such as any person might experience from time to time.
The level of anxiety referred to suggests a specific and overwhelming
experience of fear, resulting in physical symptoms or a racing pulse, and often
in feelings of impending death such as may occur in a panic attack.
Activities of daily living
2 The disability analyst considers any form of social contact including:
• Use of public transport;
• Shopping; • Talking to neighbours;
• Use of phone;
• Hobbies and interests; and
• Social interaction with family.
Mental State Examination
3 The Mental State Examination findings would be expected to reflect severe
anxiety. Rapport is likely to be poor with lack of eye contact. The customer
might be sweating and find the consultation difficult. They may be somewhat
timid in demeanour at interview. It would seem likely the person would require
a companion to accompany them to the medical examination centre due to
the high level of anxiety.
DLA Considerations
4 This Activity is most relevant to the problems that people with severe
anxiety and panic disorder might experience in the work situation or in
accessing work. Some information relating to this Activity may be helpful to
the DM in determining whether help is needed to get around. However it
should be borne in mind that the person will have significant problems in
coping with social situations arising from a diagnosed mental health disorder.
It is not intended to reflect normal feelings of anxiety or apprehension that
anyone might experience in travelling to an unfamiliar place or when meeting
new people.
Propriety of behaviour with other people – Activity 20
Descriptors
IB (a) Has unpredictable outbursts of, aggressive, disinhibited, or bizarre
behaviour, being either:
(i) sufficient to cause disruption to others on a daily basis, or
(ii) of such severity that although occurring less frequently than on a
daily basis, no reasonable person would be expected to tolerate them.
IB (b) Has a completely disproportionate reaction to minor events or to
criticism to the extent that he has an extreme violent outburst leading to
threatening behaviour or actual physical violence.
IB(c) Has unpredictable outbursts of, aggressive, disinhibited or bizarre
behaviour, sufficient in severity and frequency to cause disruption for the
majority of the time.
IB (d) Has a strongly disproportionate reaction to minor events or to criticism,
to the extent that the person cannot manage overall day to day life when such
events or criticism occur.IB (e) Has unpredictable outbursts of aggressive, disinhibited or bizarre
behaviour, sufficient to cause frequent disruption.
IB (f) Frequently demonstrates a moderately disproportionate reaction to
minor events or to criticism but not to such an extent that the person cannot
manage overall day to day life when such events or criticism occur.
IB (g) None of the above apply
Scope
1 This activity is intended to reflect difficulties in social behaviour that might be
encountered by people with psychotic illness or other conditions such as brain
injury that result in lack of insight, as well as the difficulties people with autistic
spectrum disorder may have in social behaviour. It is intended to reflect the
effects of episodic relapsing conditions such as some types of psychotic
illness, as well as conditions resulting in consistently abnormal behaviour.
“Reaction to minor events” is intended to reflect difficulties that may be
encountered by people with autistic spectrum disorder and other conditions, in
which minor adverse events causes a moderately disproportionate, or
significant reaction out with that which might normally be expected.
2 There should be clear evidence of a disorder of mental function. This may
be as a result of a specific mental illness or a condition, whether mental,
physical, or sensory resulting in cognitive or intellectual impairment.
3 An example of a strongly disproportionate reaction would be a response to
very minor criticism involving actions such as shouting, crying and storming
out of the room. E.g. a comment such as “the soup could have been warmer”
when eating the dinner prepared for them by the customer results in the
customer crying and storming out of the room.
4 A moderately disproportionate reaction would be sitting shaking and crying
in response to a minor criticism.
5 There must be evidence of mental disablement that causes a pattern of
consistent behaviour triggered in different circumstance, not just directed
towards one individual.
Activities of daily living
6 The disability analyst considers any activity involving interaction with others
where criticism may occur such as:
• Previous occupational history.
• Shopping.
• Childcare.
• Parents’ nights at school.
• Relationships with neighbours.
• Ability to cope at appointments: GP/ Hospital etc.; • Ability to cope with bills and on the phone.
• Dealing with finances and bills at the post office; and
• Appointments with official persons such as the bank manager/ social
worker/ DWP staff.
Mental State Examination
7 There is likely to be evidence of reduced insight. Cognitive function may be
impaired and evidence of addiction or thought disorder may be present.
Rapport may be poor and communication difficult.
DLA Considerations
8 People with psychotic illnesses such as schizophrenia, bipolar disorder and
those with brain injury, autistic spectrum disorder, learning disabilities and
personality disorders may have the levels of functional restriction described
under this Activity. Descriptors IB (a) to IB (e) are likely to be applicable to
customers with these disorders who require supervision and help getting
around.
Dealing with other people – Activity 21
Descriptors
DP (a) Is unaware of impact of own behaviour to the extent that:
(i) has difficulty relating to others even for brief periods, such as a few
hours; or (ii) causes distress to others on a daily basis.
DP (b) The person misinterprets verbal or non-verbal communication to the
extent of causing himself or herself significant distress on a daily basis.
DP(c) Is unaware of impact of own behaviour to the extent that:
(i) has difficulty relating to others for longer periods, such as a day or
two, or
(ii) causes distress to others for the majority of the time.
DP (d) The person misinterprets verbal or non-verbal communication to the
extent of causing the person significant distress to himself or herself for the
majority of the time.
DP (e) Is unaware of impact of own behaviour to the extent that:
(i) has difficulty relating to others for prolonged periods, such as a
week; or
(ii) frequently causes distress to others.DP (f) The person misinterprets verbal or non-verbal communication to the
extent of causing the person significant distress to himself or herself on a
frequent basis.
DP (g) None of the above apply
Scope
1 This activity is intended to reflect difficulties in social behaviour such as may
be encountered by people with a variety of conditions, including autistic
spectrum disorder, psychotic illness, and brain injury, which affect
understanding and the application of social norms of communication.
Descriptor DP (a) also includes any situation where lack of ability to self–care
and to maintain personal hygiene causes the claimant to be totally
unacceptable to other people.
Activities of daily living
2 The disability analyst considers the social interaction that occurs in:
• Social occasions;
• Relationships with friends and family;
• Previous occupations;
• Conflict with authorities or exclusion from local amenities;
• Shopping;
• Public transport; and
• Relationship with GP/ receptionists – ? frequently removed from
Practice lists etc.
Mental State Examination
3 It is likely that the customer will have very little insight into their behaviour.
Intelligence and cognitive function may also be impaired. Addictions and
thought disorder may be present. Rapport is likely to be poor when these
descriptors apply, and it may have been difficult to establish good
communication during the interview.
DLA considerations
4 In many respects the scope of this Activity relates most closely to the
problems that abnormal social behaviour described might create in the work
situation, such that effective functioning would be precluded. However the
choice of the most highly scoring descriptors DP (a) to DP(c) would indicate
the most severe disabling effects of the medical conditions mentioned above,
and may indicate a requirement for supervision.
Section 15 – Summary of ESA Mental Function
Information for DLA (table)This table is reproduced at Appendix C.
Section 16 – The Support Group and ESA 85
1 If the customer is discovered at medical examination to have a severe
illness or disability, they may fulfil the criteria for inclusion in the Support
Group. The assessment and completion of report ESA 85 is usually curtailed
in these cases. The report shows which descriptor (see below) applies to the
customer and an additional report ESA 85A is generated by LiMA justifying
the advice for the ESA DM.
2 The Support Group Activities are listed in the table at paragraph 4 below.
The disability analyst is required to choose a descriptor in only one of the
functional areas (Activities) to fulfil the Support Group (SG) criteria. Some of
the Activities mirror those in the physical/mental function assessment
described previously, when the SG descriptor represents a higher level of
functional limitation in that category e.g. reaching, manual dexterity. Other
Activities do not correlate closely and relate to different functional categories
e.g. eating and drinking, communication.
3 Although the ESA 85 report may be shorter in length in these cases, it is
likely to provide information about a customer with a severe level of functional
restriction in at least one functional category. This information may be very
helpful in determining care and/or mobility, especially if considered in relation
to other details about clinical history, typical day, clinical examination etc.
However it will be advisable to review other evidence, since the ESA 85 and
85A will not necessarily give a full account of all the disabling effects of the
medical condition. For example, in the case of a customer who cannot walk at
all because of severe lower limb pathology, there may be little information
about upper arm function or mental health.
4 Support Groups are detailed in Appendix A.
Appendix A – Support Group
Column 1
Activity
Column 2
Descriptors
1. Walking or moving on level
ground.
Cannot –
(a) walk (with a walking stick or other aid if
such aid is normally used);
(b) move (with the aid of crutches if
crutches are normally used); or
(c) manually propel his wheelchair;more than 30 metres without repeatedly
stopping, experiencing breathlessness or
severe discomfort.
2. Rising from sitting and
transferring from one seated
position to another.
Cannot complete both of the following –
(a) rise to standing from sitting in an upright
chair without receiving physical assistance
from someone else; and
(b) move between one seated position and
another seated position located next to one
another without receiving physical
assistance from someone else
3. Picking up and moving or
transferring by the use of the
upper body and arms (excluding
standing, sitting, bending or
kneeling and all other activities
specified in this Schedule).
Cannot pick up and move 0.5 litre carton full
of liquid with either hand.
4. Reaching. Cannot raise either arm as if to put
something in the top pocket of a coat or
jacket.
5. Manual dexterity. Cannot –
(a) turn a “star-headed” sink tap with either
hand; or
(b) pick up a £1 coin or equivalent with
either hand.
6. Continence –
(a) Continence other than
enuresis (bed wetting) where
claimant does not have an
artificial stoma or urinary
collecting device
(a) Has no voluntary control over the
evacuation of the bowel;
(b) Has no voluntary control over the
voiding of bladder;
(c)At least once a week, loses control of
bowels so that the claimant cannot control
the full evacuation of the bowel;
(d) At least once a week loses control of
bladder so that the claimant cannot control
the full voiding of the bladder;
(e) At least once a week fails to control full
evacuation of the bowel, owing to a severe
disorder of mood or behaviour; or(f) At least once a week fails to control full
voiding of the bladder, owing to a severe
disorder of mood or behaviour.
(b) Continence where claimant
uses a urinary collecting device,
worn for the majority of the time
including an indwelling urethral
or suprapubic catheter
(a) Has no voluntary control over the
evacuation of the bowel;
(b) Has no voluntary control over the
voiding of bladder;
(c)At least once a week, loses control of
bowels so that the claimant cannot control
the full evacuation of the bowel;
(d) At least once a week loses control of
bladder so that the claimant cannot control
the full voiding of the bladder;
(e) At least once a week fails to control full
evacuation of the bowel, owing to a severe
disorder of mood or behaviour; or
(f) At least once a week fails to control full
voiding of the bladder, owing to a severe
disorder of mood or behaviour.
(c) Continence other than
enuresis (bed wetting) where
claimant has an artificial stoma
appliance
(a) Is unable to affix, remove or empty
stoma appliance without receiving physical
assistance from another person;
(b) Is unable to affix, remove or empty
stoma appliance without causing leakage of
contents;
(c) Where the claimant’s artificial stoma
relates solely to the evacuation of the
bowel, has no voluntary control over voiding
of bladder;
(d) Where the claimant’s artificial stoma
relates solely to the evacuation of the
bowel, at least once a week loses control of
the bladder so that the claimant cannot
control the full voiding of the bladder; or
(e) Where the claimant’s artificial stoma
relates solely to the evacuation of the
bowel, at least once a week, fails to control
the full voiding of the bladder, owing to a
severe disorder of mood or behaviour. 7. Maintaining personal hygiene (a) Cannot clean own torso (excluding own
back) without receiving physical assistance
from someone else;
(b) Cannot clean own torso (excluding back)
without repeatedly stopping, experiencing
breathlessness or severe discomfort;
(c) Cannot clean own torso (excluding back)
without receiving regular prompting given by
someone else in the claimant’s presence; or
(d) Owing to a severe disorder of mood or
behaviour, fails to clean own torso
(excluding own back) without receiving—
(i) physical assistance from someone
else, or
(ii) regular prompting given by
someone else in the claimant’s
presence.
8. Eating and drinking
(a) Conveying food or drink to
the mouth.
(a) Cannot convey food or drink to the
claimant’s own mouth without receiving
physical assistance from someone else;
(b) Cannot convey food or drink to the
claimant’s own mouth without repeatedly
stopping, experiencing breathlessness or
severe discomfort;
(c) Cannot convey food or drink to the
claimant’s own his mouth without receiving
regular prompting given by someone else in
the claimant’s physical presence; or
(d) Owing to a severe disorder of mood or
behaviour, fails to convey food or drink to
the claimants own mouth without
receiving—
(i) physical assistance from someone else,
or
(ii) regular prompting given by someone
else in the claimant’s presence
(b) Chewing or swallowing food
or drink
(a) Cannot chew or swallow food or drink;(b) Cannot chew or swallow food or drink
without repeatedly stopping, experiencing
breathlessness or severe discomfort;
(c) Cannot chew or swallow food or drink
without repeatedly receiving regular
prompting given by someone else in the
claimant’s presence; or
(d) Owing to a severe disorder of mood or
behaviour, fails to—
(i) chew or swallow food or drink; or
(ii) chew or swallow food or drink without
regular prompting given by someone else in
the claimant’s presence.
9. Learning or comprehension in
the completion of tasks
(a) Cannot learn or understand how to
successfully complete a simple task, such
as the preparation of a hot drink, at all;
(b) Needs to witness a demonstration, given
more than once on the same occasion of
how to carry out a simple task before the
claimant is able to learn or understand how
to complete the task successfully, but would
be unable to successfully complete the task
the following day without receiving a further
demonstration of how to complete it;
or
(c) Fails to do any of the matters referred to
in (a) or (b) owing to a severe disorder of
mood or behaviour.
10. Personal action (a) Cannot initiate or sustain any personal
action (which involves planning,
organisation, problem solving, prioritising or
switching tasks);
(b) Cannot initiate or sustain personal action
without requiring daily verbal prompting
given by someone else in the claimant’s
presence; or
(c) Fails to initiate or sustain basic personal
action without requiring daily verbal
prompting given by someone else in the claimant’s presence, owing to a severe
disorder of mood or behaviour.
11. Communication (a) none of the following forms of
communication can be achieved by the
claimant—
(i) speaking (to a standard that may
be understood by strangers);
(ii) writing (to a standard that may be
understood by strangers);
(iii) typing (to a standard that may be
understood by strangers)
(iv) sign language to a standard
equivalent to Level 3 British Sign
Language;
(b) none of the forms of communication
referred to in (a) are achieved by the
claimant, owing to a severe disorder of
mood or behaviour;
(c) Misinterprets verbal or non-verbal
communication to the extent of causing
distress to himself or herself on a daily
basis; or
(d) Effectively cannot make himself or
herself understood to others because of his
disassociation from reality owing to a
severe disorder of mood or behaviour.
Appendix B- Comparison ESA 85 (WCA) with IB
85 (PCA) for the Physical Activities
Activity Differences
compared to IB 85
ESA 85 Significance of
change & notes
Walking Descriptors W(e) &
W(f) removed –
cannot walk more
than 400 metres
(& 800 metres
respectively)
without stopping
or severe
Descriptors added –
W (c) – cannot walk
up or down 2 steps
even with the
support of handrail.
W(d) – cannot walk
Both refer to
walking with stick
or other aid if
normally used.
50 and 100 metre
delineations
provide more discomfort more than 100
metres without
stopping or severe
discomfort
clarity in respect of
‘virtually unable to
walk’
Ability to manage
stairs incorporated
into this Activity
Walking up
and down
stairs
No separate Stairs
Activity in ESA 85
Stairs – covered by
descriptor W(c) see
above and other high
descriptors in the
Walking category
If customer
virtually unable to
walk, always need
to consider
whether they have
difficulty on stairs
Sitting Not a separate
Activity in ESA 85.
In IB 85 separate
Activity with 5
descriptors
describing ability to
sit comfortably
without having to
move because of
discomfort
Incorporated into the
new Activity Standing
and Sitting as 2
descriptors S(b) &
S(f) – cannot sit in a
high back chair for
more than 10
minutes ( 30
minutes
respectively) before
needing to move
from the chair
because the degree
of discomfort
experienced makes
it impossible to
continue sitting.
These sitting
descriptors not of
direct relevance to
DLA; more
applicable to the
work situation
Rising from
sitting
Not a separate
Activity in ESA 85.
In IB 85 separate
Activity with 4
descriptors
Incorporated into the
new Activity Standing
and Sitting as 2
descriptors S (c) –
cannot rise to
standing from
sitting in an upright
chair without
physical assistance
from another person
and S (d) – cannot
move between one
seated position and
another seated
position located
next to one another
without receiving
physical assistance
Indicate cases
where help need to
rise from a chair
and in wheelchair
transfers.
Note refers to an
upright chairfrom another person
Standing Not a separate
Activity in ESA 85.
In IB 85 separate
Activity with 7
descriptors
Incorporated into the
new Activity Standing
and Sitting as
descriptors S (a) –
cannot stand for
more than 10
minutes, unassisted
by another person,
even if free to move
around, before
needing to sit down
and S(e) cannot
stand for more than
30 minutes, even if
free to move
around, before
needing to sit down.
Under ESA
regulations
someone who can
stand with 2 sticks
is considered to be
able to stand
Standing
and Sitting
ESA 85 Activity –
combines 3
activities that are
evaluated
separately in IB 85
Clinical findings,
observations and
daily activities
more logically
considered and
presented together
in report.
Bending
and
Kneeling
Descriptor B(c)
removed –
sometimes cannot
either, bend or
kneel, or bend and
kneel as if to pick
up a piece of
paper from the
floor and
straighten up
again
Descriptors added –
B(b) – cannot bend,
kneel or squat, as if
to pick up a light
object, such as a
piece of paper,
situated 15 cm from
the floor on a low
shelf, and to move it
and straighten up
again without the
help of another
person
B(c) – cannot bend,
kneel or squat, as if
to pick up a light
object off the floor
and straighten up
again without the
help of another
person
Removes the
difficult to define
time scale of
‘sometimes’.
ESA Activity
describes the
function being
evaluated more
clearly.Reaching Descriptors RS (e)
& RS(f) removedRS(e) – cannot rise
one arm to head
as if to put on a
hat but can with
other
RS (f) – cannot
rise one arm to
head as if to reach
for something but
can with other.
Descriptors R(a),
R(b), R(c) & R (d) all
refer to inability to
raise either arm.
Descriptors refer to
customers with
bilateral
impairment(s). This
is a greater degree
of functional
restriction than in
the PCA
Picking up
or moving
or
transferring
objects
Replaces Activity
known as Lifting &
Carrying in IB 85
5 descriptors
removed :-
MH(a) – Cannot
pick up a
paperback book
with either hand
MH© – Cannot
pick up and pour
from a full
saucepan or kettle
of 1.7 litre
capacity
MH(d) – Cannot
pick up and carry
a 2.5kg bag of
potatoes with
either hand
MH(e) – Cannot
pick up and carry
a 0.5 litre carton
of milk with one
hand but can with
the other
MH(f) – Cannot
pick up and carry
a 2.5kg bag of
Descriptors added
P(a) – Cannot pick
up and move a one
litre carton full of
liquid with either
hand.
P(c) – Cannot pick
up and move a light
but bulky object
such as an empty
cardboard box,
requiring the use of
both hands together
Descriptors refer to
customers with
bilateral
impairment(s). This
is a greater degree
of functional
restriction
compared to the
PCA.
The weights used
in ESA are lighter
and are more
applicable to DLA
personal care and
meal preparation.potatoes with one
hand but can with
the other
Manual
dexterity
Descriptor D (e)
removed: – cannot
tie a bow in laces
or string
Descriptors added
M(e) – Cannot
physically use a
conventional
keyboard or mouse
M (f) – Cannot do
up/undo small
buttons, such as
shirt or blouse
M (i) – Cannot pour
from an open 0.5
litre carton full of
liquid.
More emphasis on
use of both hands
to carry out the
functions, and
therefore more
applicable to DLA
personal care and
meal preparation.
Ability to use a
keyboard or mouse
shows importance
to work related
activities in ESA.
Vision Descriptors V (a) &
V (b) removed:-
V (a) – cannot tell
light from dark
V(b) – cannot see
the shape of
furniture in the
room.
Descriptors added
V(A) – cannot see at
all
V(c) – has 50% or
greater reduction of
visual fields.
V(e) – has 25% or
more but less than
50% reduction of
visual fields.
ESA evaluates
both visual acuity
and visual fields,
and therefore
provides a more
detailed
assessment of
visual impairment.
More useful
information in
respect of work
capability and how
a customer
manages tasks of
daily living
including ability to
get around.
Hearing Descriptors H(b) &
H (e) removed:-
H(b) – cannot hear
well enough to
follow a television
programme with
the sound turned
up
H(e) – cannot hear
Descriptor added
H (d) – cannot hear
someone talking in
a loud voice in a
busy street,
sufficiently clearly
to distinguish the
words being
spoken.
Evaluated with
hearing aids, if
normally worn.
Report likely to
contain information
about people with
profound hearing
impairments, and
therefore of more
use in DLA claims.well enough to
understand
someone talking
in a normal voice
on a busy street
Speech Descriptor SP (b)
removed: – speech
cannot be
understood by
family or friend
Remaining
descriptors
unchanged
No significant
change.
Continence Activity subdivided
under 3
headings10(a),
10(b) and 10(c):-
10 (a) Continence
other than
enuresis (bed
wetting) where the
claimant does not
have an artificial
stoma or urinary
collecting device.
10 (b) Continence
where the
claimant uses a
urinary collecting
device, worn for
the majority of the
time including an
indwelling
urethral or
suprapubic
catheter.
10 (c) Continence
other than
enuresis (bed
wetting) where the
claimant has an
artificial stoma.
See main text for
full details of
individual
descriptors.
10 (a) Evaluates if
customer has urinary
and/or bowel
continence and how
frequently.
10(b) Relates to use
of urinary collecting
devices and whether
help is needed to
manage these.
10(c) Relates to
individuals with an
artificial stoma and
whether they need
help to manage it.
Although
presentation of
information in this
Activity appears
complex, the
nature and effects
of incontinence are
identified.
People who need
help with
incontinence
devices are clearly
identified.
Remaining IB 85 Activity is ‘ ESA 85 Activity is Less detailed conscious Remaining
conscious without
having epileptic or
similar seizures
during waking
moments’
3 descriptors
removed:-
F(a) – has had an
involuntary
episode of lost or
altered
consciousness at
least once a day
F ( e) – has had an
involuntary
episode of lost or
altered
consciousness at
least once in the
last 6 months
F(f) – has had an
involuntary
episode of lost or
altered
consciousness
once in the last 3
years
‘Remaining conscious
during waking
moments’ and the
descriptors refer to
‘lost or altered
consciousness,
resulting in
significantly disrupted
awareness or
concentration’ and the
3 descriptors
attracting a score
are:-
F (a) – ……..at least
once a week
F (b) – ……….at least
once a month
F (c) – ………at least
twice in the last 6
months ….
information about
the frequency of
episodes, but time
intervals are more
applicable to work
related activities.
Applies to
generalized &
partial epileptic
seizures including
absence seizures
(petit mal), and
also cardiac
arrhythmias and
hypoglycemia.
Scope of medical
conditions that
may be included
appears to be
wider than PCA
Appendix C – Summary of how to use ESA 85
Mental Function Information
DLA
Considerations
Mental Health
Functional
Activity
Relevant Descriptors Metal health
disorders
Learning or
comprehension
in completion
of tasks
(Activity 12)
LT (c),LT (d) & LT (e) Learning
disabilities,
dementia,
brain injury.
Preparing a main
meal
Memory and
concentration
(Activity 14)
MC (a), MC(b) & MC
(c)
Learning
disabilities,
dementia, brain injury,
depression,
anxiety,
schizophrenia
Execution of
tasks (Activity
15)
ET(a), ET(b), ET(c) &
ET(d)
Learning
disabilities,
dementia,
brain injury,
depression,
anxiety,
schizophrenia,
obsessivecompulsive
disorder.
Initiating and
sustaining
personal action
( Activity16)
IA(a), IA(b),IA(c) &
ID(d)
Depression,
schizophrenia
Awareness of
hazard (Activity
13)
AH(a) & AH(b) Learning
disabilities,
dementia,
brain injury.
Learning or
comprehension
in completion
of tasks
(Activity 12)
LT(a),LT(b),LT(c),LT(d)
& LT (e)
Learning
disabilities,
dementia,
brain injury
Memory and
concentration
(Activity 14)
MC (a), MC(b) & MC
(c)
Learning
disabilities,
dementia,
brain injury,
depression,
anxiety,
schizophrenia
Execution of
tasks (Activity
15)
ET(a), ET(b), ET(c) &
ET(d)
Learning
disabilities,
dementia,
brain injury,
depression,
anxiety,
schizophrenia,
obsessivecompulsive
disorder.
Attention/prompting
– self-care,
avoidance of selfneglect,
maintenance of
nutrition, hydration.
Initiating and
sustaining
IA(a), IA(b),IA(c) &
ID(d)
Learning
disabilities, personal action
( Activity16)
dementia,
brain injury,
depression,
schizophrenia
Learning or
comprehension
in completion
of tasks
(Activity 12)
LT(a),LT(b),LT(c),LT(d)
& LT (e)
Learning
disabilities,
dementia,
brain injury
Memory and
concentration
(Activity 14)
MC(a), MC(b) & MC (c) Learning
disabilities,
dementia,
brain injury,
depression,
anxiety,
schizophrenia
Awareness of
hazard (Activity
13)
AH(a) & AH(b) Learning
disabilities,
dementia,
brain injury
Proprietary of
behaviour with
other people
(Activity 20)
IB(a), IB(b) & IB(c) Learning
disabilities,
brain injury,
autistic
spectrum
disorder
Supervision
Dealing with
other people
(Activity 21)
DP(a),DP(b) & DP(c) Learning
disabilities,
brain injury,
autistic
spectrum
disorder,
psychotic
episodes
Getting around
(Activity 18)
GA(a), GA(b), GA (c) &
GA (d)
Learning
disabilities,
dementia,
brain injury
agoraphobia,
severe anxiety
Awareness of
hazard (Activity
13)
AH(a) & AH(b) Learning
disabilities,
dementia,
brain injury.
Getting around
Proprietary of IB(a), IB(b), IB(c), IB(d) Learning behaviour with
other people
(Activity 20)
& IB(e). disabilities,
brain injury,
autistic
spectrum
disorder
Dealing with
other people
(Activity 21)
DP(a), DP(b),
DP(c),DP(d), DP(e) &
DP(f).
Learning
disabilities,
brain injury,
autistic
spectrum
disorder,
psychotic
episodes
Appendix D Comparison of roles undertaken by
clinicians and disability analysts
Clinician Disability analyst
Role Makes diagnosis and treats • Assesses
• Impairment
• Functional
limitations/restrictions
• Disability
How History
• Tends to take what
patient says at ‘face
value’
• Concentrates on
symptoms
Examination
• Tends to take
findings at ‘face
value’
• Usually ignores
informal
observations
History
• Accepts diagnoses from
clinician
• Brief history of medical
condition
• Symptoms
• Asks how medical condition
affects function
• Daily living activities
• Looks for consistency in
overall picture
Examination
• Informal observations (often
very important)
• Objective clinical examination
• Looks for consistency and
inappropriate signs (i.e.
findings not indicative of
disease)Specific
skills
Diagnostic techniques
(special tests)
Detailed knowledge of
treatments
Objective assessment of disability
Opinion fully justified
Knowledge of legal framework when
giving advice
Other Usually the patient’s
advocate
• Acts in patient’s beat
interest
• Maintains
doctor/patient
relationship
Not acting as patient advocate
• Gives objective advice in
accordance with law
• Advice based on detailed
functional assessment

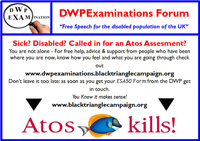
4 Responses
Get the Tories Out they are Toff Scum
It Absolutely makes my Blood Boil with Rage
So they are now using ESA to define if you are eligible for DLA if you are a new applicant. Or is this the new plan on the move over to PIP, well no as pip has very few decriptors and is designed to exclude rather than include. It is purely an anti disability cost cutting and lining pocket of rich exercise. They just seem to want to make it harder for people to claim money that is rightfully theirs in my opinon.
well i am an aspie,i wont fit most of these,this is just done to deny disability to save money to give in pre election give away,i hope the public can see this .. jeff ..
I love the way the final section compares the abilities of doctors/clinicians and disability analysts. So doctors only take things at face value and take findings at face value do they?? Ok so next time I see my GP I’ll just tell him I’ve got malaria and he’ll take my word for it. Ridiculous.