 An independent review of workplace health has suggested a key role for occupational health in addressing the UK’s sickness absence problem. Nic Paton reports.
An independent review of workplace health has suggested a key role for occupational health in addressing the UK’s sickness absence problem. Nic Paton reports.
In December 2007, Occupational Health magazine described Dame Carol Black’s groundbreaking Working for a Healthier Tomorrow review of workplace health as a “once-in-a-generation opportunity” and an “early Christmas present for OH practitioners everywhere”.
This time, in conjunction with former director general of the British Chambers of Commerce, David Frost, her latest report, Health at work – an independent review of sickness absence, has emerged once again in the run-up to Christmas and, again, it appears as a case of Black bearing gifts, at least potentially, for the profession.
Prime Minister David Cameron set the review in motion in February 2011, with a remit to “explore radical new ways on how the current system can be changed to help more people stay in work and reduce costs”, as well as feed into the Government’s ongoing reforms of welfare – especially getting people off benefits and back into work – and employment regulation and red tape.
The result is a wide-ranging bundle of recommendations (see panel), some of which, particularly the creation of an Independent Assessment Service (IAS) to assess and rehabilitate people back into work, have the potential to offer significant opportunities for occupational health practitioners in terms of leadership, delivery and implementation.
Best for the job
As Dr Sayeed Khan, chief medical adviser for the manufacturers’ organisation EEF, points out, while there will be many Is to dot and Ts to cross, it is clear that the model as set out by Black and Frost plays very much to OH’s strengths.
“The devil, as ever, is going to be in the detail. Who, for example, is going to run the IAS? In the report, it speaks about occupational therapists and other healthcare professionals, which I wouldn’t object to, but I do think occupational health professionals will be needed too, perhaps in terms of overseeing things. Occupational health will have a crucial role to play in this,” he says.
“There will be standards that will need to be sorted out and quality assurance, and simply ensuring the service is fit for purpose. But it could be a real opportunity for a lot of OH professionals,” he adds.
The report states: “In an ideal system, people who are unable to work would be swiftly identified and supported; those with conditions that are compatible with their current work would receive early treatment and support to return [to work] quickly; and those needing to change jobs would be efficiently helped back into work. Costs would be fairly distributed between employers, individuals and the state, and incentives aligned to manage these costs. For some people, the current system falls well short of this ideal at every stage of the journey.”The report itself makes it very plain that the UK’s current sickness absence management system, if not exactly broken, certainly is not in rude health.
Absence costs
In a climate where, the report estimated, employers pay out £9 billion per year in sick pay and associated costs (not to mention indirect costs), a system where someone who is signed off work is automatically deemed completely unfit to work is a blunt instrument, the document recognises.
“Unless this is addressed, employers cannot make adjustments to help people whose illness is compatible with a return to work. Solving this issue is the first crucial step in stemming sickness absence and inactivity. In longer-term and more difficult sickness cases, employers have told us that they need independent, bespoke advice, especially if they do not have their own OH services. Such advice could help doctors, who usually do not consider themselves expert in this area,” the report advises.
To this end, it is intended that the IAS will provide an in-depth assessment of an individual’s physical and/or mental function, as well as advice about a supported return to work, and this will normally be triggered by an absence of about four weeks. The service, Black and Frost argue, could save employers £100 million per year in sickness costs and benefit the economy to the tune of £150 million per year.
The report is also critical of the management by employers of long-term absence, which it argues is “uneven”, in large part because of disparities in access to occupational health.
“Larger employers and those in the public sector are more likely to offer occupational health services. Higher earners are individually more valuable to employers and often have readier access to private healthcare. Consequently, employees who earn less and are less qualified, and those from smaller firms, are more likely to be excluded from interventions to get them back to work. They are, therefore, more likely to fall on to state benefits,” the report advises.
To this end, investment by employers in medical treatments or vocational rehabilitation should attract tax relief, the report recommends, with this targeted at basic-rate taxpayers.
This, it estimates, would cost the Treasury around £150 million per year but would result in up to £250 million in gains to employers, which is important given the Treasury’s long-standing opposition to such incentives.
Similarly, it recommends the abolition of record-keeping obligations under statutory sick pay, something it calculates could save employers £44 million per year.Other recommendations include abolishing the Percentage Threshold Scheme (PTS), under which employers that experience high rates of sickness absence can be compensated by the Government, with the argument here being that the scheme costs £50 million per year, yet gives employers no incentive to reduce absence.
More widely, the report recommends the establishment of a free “job-brokering” service for anyone with a sickness absence period of 20 weeks or more, possibly delivered through the Department for Work and Pension’s existing Work Programme.
This, Black and Frost calculated, could save the state up to £300 million per year and increase economic output by £800 million per year. The report’s recommendations as a whole could, the authors argue, save employers £400 million per year, the state up to £300 million per year and boost economic output by up to £1.4 billion.
Investing in occupational health
Reaction from employers’ groups and the occupational health profession has been, by and large, positive, albeit not without some further questions being posed.
Along with who is going to lead the IAS, there are the questions of, first, how will the IAS fit with (or even replace) a Fit for Work Service, something that is still being evaluated by the Government, with conclusions due in 2013? And, second, whether or not it could inadvertently prompt employers to conclude that, if the state is going to offer this anyway, why should they bother paying for an OH service themselves?
“Are some employers going to bail out from having an OH service, whether in-house or contracted? That could of course be an unintended consequence. There is a risk that, under the IAS, employers turn around and say: do I need my own OH service anymore?” recognises EEF’s Khan.
However, Ben Willmott, head of public policy at the Chartered Institute of Personnel and Development, believes organisations that have already taken the plunge and are seeing benefits will be unlikely to change just for change’s sake.
“I would be surprised if firms cut their existing OH investment. If you have an OH service, it will be providing a bespoke service dovetailed to your needs and manned by people who have knowledge and awareness, the IAS will not have that advantage. If the business case is clear and they are seeing return on investment, then why would you get rid of it?” Willmott argues.
The wider challenge will be how to reach out to those businesses that have not yet seen or understood the business case to invest in occupational health.
“For some, it can be quite a leap of faith, and I suspect the IAS will help to widen that understanding, the potential value of accessing something like occupational health,” he adds.
Leading roles
Another question that may be asked is: will occupational health, whether physicians, nurses, advisers or technicians, even have the capacity to take a lead role, given the size of the profession?
“The new assessment service will have to include increased access to occupational health specialists. Occupational health will, I feel, need to become a mainstream speciality available to all GPs,” argues the president of the Society of Occupational Medicine, Dr Henry Goodall.
Many private providers already have experience in offering case-management services, so there could be opportunities there, while for individual occupational health practitioners with the right skills, there could also be opportunities to work more closely with, say, GP practices, argues Graham Johnson, clinical lead – nursing, at Bupa Health & Wellbeing.“One answer might be a fast-track occupational physician training programme, so, rather than training everyone to the same level of experience over four years, there is an option of a shorter, sickness-absence-management-based training, as well as looking at prevention, wellness, lifestyle, health coaching and so on,” he adds.
“This, as I recall, was something mooted a few years ago but never really came about, but, as GPs are now becoming budget holders they may decide that they want to make that sort of investment if they can access an OH adviser with the relevant skills. So there could be opportunities there,” he suggests.
Opportunity knocks
Generally, the report is “a marvellous opportunity” for occupational health, agrees Anne Harriss, course director for occupational health nursing at London’s South Bank University, particularly in terms of the emphasis that it gives to early intervention.
“My main disappointment is that there is no emphasis on companies setting up their own OH services. It had an opportunity to recommend that it be made mandatory for firms either to have something in-house or plug into a consultancy,” she says.
“I like the job-brokering service and the recommendation that complex cases need to be processed more quickly. The idea of tax relief for vocational rehabilitation is brilliant but it would have been good to make the same suggestion for OH services,” she adds.
Finally, and lest we all get too carried away, there is also the small question of whether or not the Government will agree to all, or any, of this in the current straitened financial climate.
Its record, to be fair, is relatively positive, given that, first, it quickly committed to the development of a Fit for Work Service and, second, set this review in motion in the first place, with welfare reform minister Lord Freud giving the findings an initial welcome.
Moreover, the report does, as was intended, dovetail with the Government’s welfare reform/cost-saving agenda and makes a compelling case for upfront investment leading to greater long-term savings.
Nevertheless, we may not know the answer for some time. The “rumour” is that ministers are likely to take their time before coming back with their considered response, with six months being mooted as a probable timeframe, although, officially, the line is simply “during 2012”.
For occupational health professionals, however, the wait could well be worth it, as long as the profession is able to rise to the challenge.
As Johnson argues: “Overall, this is definitely a move in the right direction; it is yet another thing that puts occupational health on the map, another opportunity to demonstrate what we can do in terms of employee health and wellbeing. So if occupational health does not grasp this, it only has itself to blame.”
|
The Government should fund a new Independent Assessment Service to provide an in-depth assessment of an individual’s physical and/or mental function. This would provide advice about how an individual on sickness absence could be supported to return to work and should come into play after a person has been off for four weeks. The Government should revise the fit note guidance to ensure that judgments about fitness to work move away from only job-specific assessments. The Government should do more to improve knowledge and awareness among healthcare professionals, particularly those involved in certification, of the Work Capability Assessment (WCA) and the benefits system generally, plus the importance of work for health. Expenditure by employers targeted at keeping sick employees in work (or speeding up their return to work), such as medical treatments or vocational rehabilitation, should attract tax relief. This should be targeted at basic-rate taxpayers. Existing tax relief on employee assistance programmes should be retained. The Government should abolish the Percentage Threshold Scheme, which compensates mostly smaller employers for very high rates of sickness absence in their organisations, but (the report argues) reduces incentives to manage absence. Record-keeping obligations under statutory sick pay should be abolished, thereby helping to reduce employer administrative burdens. The Government should update its “Employers’ Charter” to address misconceptions around sickness absence management, especially legal uncertainty. The Government should carry out further research into the reasons behind the significant number of people claiming ill-health benefits who come straight from work, especially from smaller employers, but appear not to have been paid sick pay by their employer beforehand. Public sector employers should take immediate action to bring the worst performing parts of the public sector up to the standards of the best. The Government should also review occupational sick pay in the public sector. A new job-brokering service should be introduced to help long-term sick employees find new work (where appropriate) before they fall onto the benefits system. This service should be offered free by the state in cases of very long-term absence (at 20 weeks or sooner), but should be available earlier for individuals and employers willing to pay for it. The Government should consider delivering this service as an extension of the Department for Work and Pensions’ Work Programme. The Government should end the employment support allowance (ESA) assessment phase altogether. People should go onto ESA only if they qualify after a WCA or, as at present, if they qualify to pass directly onto ESA without a face-to-face WCA. This recommendation, in turn, should be supported by changes to Jobcentre Plus’s claims policies and processes to prevent large numbers of people being inappropriately directed towards ESA. (Our italics – BTC) |
|
|
Industry views |
|
|
James Freeston, sales and marketing director, AXA PPP: “Dame Carol Black and David Frost have made some bold, constructive recommendations which, if introduced, should significantly improve sickness absence management in Britain. “As a provider of employee health and wellbeing support services, naturally we welcome their proposals for tax relief for targeted employer-funded vocational rehabilitation of ill or injured basic-rate-taxpayer employees. We further support the authors’ recommendation that employer-funded psychological support services (counselling) to help employees to deal more effectively with the pressures in their lives should not be taxed as a benefit in kind.” Helen Hargreaves, senior policy and research officer, Chartered Institute of Payroll Professionals (CIPP): “The CIPP is very disappointed by the suggestion to scrap the Percentage Threshold Scheme. By the Government’s own admission, in 2009-10 over 90% of claims were from smaller businesses and averaged less than £500 per claim. The Percentage Threshold Scheme, in our opinion, does not deter employers from managing sickness absence, it simply helps them meet some of the cost of that absence. “We are also confused by the suggestion that abolishing the record-keeping obligations for SSP will save employers an estimated £44 million. As employers will still need to keep records of SSP for other business obligations, it is unclear how these savings will be achieved.” John Longworth, director general of the British Chambers of Commerce: “The existing fit note system does not work for business. Since employers want individuals back in the workplace as soon as they are able, the proposal for a thorough assessment at four weeks will boost employer confidence. Most people who are off sick could undertake some duties, so the new system will get them back into work sooner, benefiting individuals, businesses and the economy as a whole. “The review was right to discount compulsory insurance, which would not tackle the problem of sickness absence in British companies, and simply added more costs for all concerned. Ministers must focus on implementing the new assessment and the other measures recommended by this review quickly, to make sure everyone who can work, does work.” Catherine McLoughlin, chair, UK Rehabilitation Council: “Our best employers are world class when it comes to rehabilitation, but there aren’t enough of them. It doesn’t matter what other good things the Government does, the sickness absence review will only work if it addresses the question of how to make our rehabilitation outcomes as good as those of other modern economies. “This means engaging the workplace and public in promoting the most effective rehabilitation and not just assuming the state will take care of it. Money invested in rehabilitation very quickly more than pays for itself through increased productivity and reduced reliance on benefits. |
|
One response
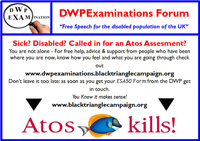
When I was struggling in work, OH helped me tremendously.They supported me to take as long as I needed off and “shoved” management into being supportive and formulating effective back to work plans. They recommended retirement on health grounds with highest level of pension, after years of helping me stay in work with a chronic illness, when my condition deteriorated.They respected my wishes helping me to stay in work as long as I could…and surprisingly this was ATOS but not the same arm as those that undertake the abysmal WCA.
These recommendations will just take all these supportive measures away by introducing WCA not related to job (this is about your specific job though) and “job brokerage” (which we know does not work from organisations like A4E) into the workplace. It will not help people stay in work as long as possible but will stop them receiving ESA when sacked at an earlier stage and taken off benefits all together when their contributory JSA runs out even earlier-get employers to pay for OH that says they are fit for some kind of work the employer can’t provide, sack them and because they have been assessed as fit for some kind of work the govt can save on the welfare bill. It also insures a lot of ATOS contracts, as they have developed the LiMA system which can now be used inappropriately in the workplace. This will not help workers, employers or OH but will lesson welfare cost for govt and make a lot of extra money for ATOS and back to work companies who have shown to be ineffective on all measures other than raiding the public purse.