Community mental health teams are having to spend an increasing amount of time helping service users claim benefits
The Masked AMHP, Guardian Professional,

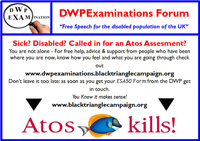
More support is needed for work capability assessments, as a result of planned changes to benefits for disabled people. Photograph: David Sillitoe for the Guardian
Professionals working in community mental health teams have ever increasing work pressures. The current changes to the NHS and local authorities mean mental health patients are “clustered” according to their symptoms as the means of obtaining funding for mental health trusts.
This is alongside the freezing of vacant posts and plans to cut back up to 20% of the clinical workforce. All of this leaves less time available for face to face contact with service users.
I am a social worker in a community mental health team. One part of my job is to advocate on behalf of the service users with whom I work. Sometimes this just involves signposting – for instance, referring them to the local citizens’ advice bureau for advice on benefit problems, or involving a housing advice worker if they have housing problems.
Increasingly, however, I am having to help people not just to claim the benefits to which they are entitled, such as disability living allowance (DLA) or employment and support allowance (ESA), but also to help prevent them having those benefits withdrawn.
With the planned changes to benefits for disabled people, such as the replacement of DLA with the personal independence payment, more people with disabilities will need specialist advocacy services. This is at the same time as funding is being removed from organisations such as Citizens Advice.
Ideally, the agencies that assess and review people’s benefits would have an understanding of individuals’ problems and disabilities, and provide a process that would produce a true picture of their ability or otherwise to work.
Unfortunately, the current assessment process seems to be explicitly designed to reduce the number of successful claimants.
Rosa is a good example of this. Rosa has schizophrenia. When she is unwell, she can become dangerous, as she focuses her paranoid delusions on casual acquaintances or strangers. She will then stalk them, sometimes breaking into their homes. In the past, she has been arrested and has even spent time in prison because of this.
She has had several acute hospital admissions over the years, often for several months at a time. Even when she is well enough to be discharged, she remains disabled by the negative symptoms of schizophrenia – lethargy, lack of motivation, concrete thinking, and difficulty adapting to change.
The other day I took Rosa to her work capability assessment, which she must attend in order to receive employment and support allowance. It was 30 miles away from where she lives. I had to take her to the assessment, as she would be unable to manage to get there herself, and then I had to actively participate in the assessment itself. This took half a day.
The assessment itself takes 30 minutes or more. The assessor asks a range of questions relating to what the person can and cannot do, and the assistance they need in activities of daily living. Questions are asked about the effects of the condition, about medication, and what they like to do.
The last time Rosa went to an assessment (I took her there, but made the mistake of waiting outside), she glossed over or denied her disabilities, as she does not realise she has them. These assessments do not seem to be geared up for accurately assessing people with “invisible” disabilities such as mental illness.
As a result, she was put onto jobseeker’s allowance, having been assessed as being capable for work. This resulted in a reduction in her benefits and the added stress of attending work focused interviews. This pressure resulted in a relapse in her illness and another extended hospital stay.
Unfortunately, if we don’t take people like Rosa to their assessments, they would be at risk of losing their benefits; that would have a potentially disastrous effect on their mental health, which in turn could lead to further acute hospital admissions.
There’s a perfect storm brewing.
The Masked AMHP is a social worker in a community mental health team in rural England and has been an approved mental health professional since 2007

No responses yet