Michael Kamalarajan, consultant in elderly medicine, scans his eyes down the list of 28 patients and wonders who he can send home. He runs through the names from another era – Beryl, Florence, Ivy, Una, Winifred, Frederick, Raymond, Albert, Cyril, Walter, Margaret, Olive – searching for someone who might be ready to be discharged.
It’s a frustrating morning meeting. The locum doctor is running behind, the occupational therapist is on long-term sick leave and the physiotherapist is not on rota to work today, which makes it challenging to get the documents in place so patients can be cleared to leave.
“Edith is getting better, but we need to sort out somewhere for her to go,” the ward nurse says. “Dinah is waiting for her assessment. There’s no medical reason why she should be staying.”
A social worker needs to spend time with another patient to calculate how home care visits should be arranged and paid for, the occupational therapist needs to meet the man in the next bed to work out how much he can do for himself. The appointments keep getting delayed, and the patients remain bedbound in this busy, cluttered ward, curtains drawn against the sun, bottles of blackcurrant squash on their tables.
Dr Kamalarajan’s patience gradually evaporates. “This is irritating and confusing. I said he is ready to go home,” he says, when the paperwork for another patient is found to be still incomplete.
These problems represent the irksome reality that gets in the way of attempts to improve hospital efficiency. With hospitals under pressure to save money, everything comes down to beds and the length of time that patients linger in them. Heartlands hospital in east Birmingham is one of the busiest hospitals in the country and, like all hospitals, it is undergoing a period of profound uncertainty. The NHS reform proposals have so far focused less on hospital management, but all hospitals across the country are committed to radical cost-cutting at a time when demand for their services is soaring.
Although the coalition promised to protect the health budget, expenditure on the NHS will be flat in real terms until 2015. The service will find this challenging; since it was founded, the NHS has averaged increases in real terms of 4% a year, and 7% since the turn of the century. To ensure that the rising demand for services is met, without damaging quality, at a time of frozen budgets, the NHS is committed to finding £20bn worth of savings by 2015. The preexisting so-called Nicholson challenge, named after NHS chief executive, Sir David Nicholson, already required individual hospitals to make unprecedented savings.
The Heart of England Trust, which embraces three hospitals across Birmingham including Heartlands, is committed to shaving 4% from its £600m annual budget – equivalent to £24m – every year over that period, and expects to cut 1,600 posts out of the total headcount of around 10,000.
The easiest way to reduce spending without affecting services is to shorten the time each patient spends inside the building. The hospital management’s vision for how to do that is focused on diverting large numbers of patients to clinics elsewhere, before they are admitted, and sending those who are admitted home as quickly as possible.
It seems a happy solution because it will both cut costs and prove better for patients, for whom extended hospital stays bring the risk of infection, pressure-sores and institutionalisation.
This is particularly important in the elderly care service, where people are living longer with expensive chronic conditions such as diabetes, heart failure and dementia. Pressure on services is intensifying (adding an extra £1bn a year to NHS costs, according to the thinktank the King’s Fund). If the hospital can swiftly usher patients out of the building, it can shut down wards, a process that the hospital chief executive, Mark Newbold, sees as a sign of success.
“The real breakthrough in terms of reducing staff is when you reduce capacity. So if we can close a ward, then we don’t need those staff, and no one will notice that those staff aren’t there because that facility is not open,” Newbold says.
However, reality throws up obstacles to this plan. Because social services budgets are being cut at the same time, delays beyond the control of hospital staff slow the flow of patients back into the community.
Kamalarajan believes that hospitals are not the right place for a lot of the elderly people confined there, but he is worried that the parallel cuts to services outside the building will make it hard for the idea to work.
Of the 28 patients on the ward this morning, he thinks eight were medically ready to go home, but couldn’t leave because their next move was uncertain. The RTL (ready-to-leave) column on the ward whiteboard has not been filled in because of a staffing shortage.
“There should be dates here, but none of them are filled in, which means our efficiency has gone down,” he says. “If one person is off on the nursing/admin side, there is no time to do this – everyone else is too busy.”
His department has been given a clear target for savings. “The only way we can actually do this is to shut more beds. To shut more beds we need to bring the length of stay down and look for other ways of managing patients so that they are not clinically neglected. The way we are trying to do this is by not admitting patients who don’t need the higher technology of the hospital. But you need to support them in their own homes. Unless there is a parallel investment into the community resources, then it will be impossible.”
The cost of a mattress
Among staff in the department of elderly medicine there is a sense that cost-cutting is going to become more urgent in the near future, but they are only beginning to feel it. Already they are more money-conscious than they might have been 10 years ago, and the cost of everything is impressed on junior workers.
Bev Baker, senior sister in the acute stroke unit, is trying to make nurses understand the true costs of the beds that patients lie on. Not just the average figure of around £300 per bed per overnight stay, but the precise cost of every aspect of that stay, down to renting the mattresses from the internal supplies centre. She has printed out information sheets for nurses: a basic overlay mattress will cost £5.60 a night, a bi-wave mattress (a bit like a lilo) costs £7.60, a Trinova mattress (that you might use for a fragile, malnourished patient) £9.60 and an Arrow bed – which can be lowered to the floor and used for people at risk of falling out of bed – costs £12.
“Our mattress budget for a ward of 34 people is £32,280 a year – £2,690 a month,” she says. “We’ll be told by an accountant every week if we’ve spent too much on mattresses, so we’re telling nurses: step down the mattresses where possible.”
A new cost-consciousness is prevalent. “Twenty years ago, people might have opened a packet of swabs to mop up spilled tea – no one would do that now; nurses know that a catheter costs £40, and which type of medical tape is expensive,” she says.
Along the corridor, in the stroke rehabilitation ward, nurses have organised staff discos and cake sales to buy new equipment. The senior sister, Julia Melton, explains that if she were to try to buy new monitoring equipment – to measure pulse and blood pressure – of the sophisticated variety that the cake sale recently funded, she would have to dip into her weekly budget, money that is already tightly stretched to buy stores. She points out boxes of incontinence nappies in the stockroom; the pads cost £11 for a box of 28. “Patients need five pads a day when they are incontinent as a result of a stroke,” she says.
Elderly care, she says, has never been as glamorous as cancer and heart departments, so gets less funding from drug companies and charities, forcing nursing staff to take fundraising matters into their own hands.
The way stroke treatment is managed has been totally reorganised over the past few years to ensure that patients get specialist treatment fast, before moving on to rehabilitation. But Melton notes that the apparent pressure to get people out of the acute wards into rehabilitation wards and on their way home as fast as possible appears to mean that patients are brought into her ward before they are well enough to benefit from the rehab services.
“Stroke is the third biggest killer and it is the most disabling physically and mentally. Most of our patients are not the people that they were before they had the stroke . . . They can’t walk any more, they have swallowing problems, understanding problems,” she says. Usually they stay for several weeks, relearning how to walk upstairs, or getting help from speech therapists, but today two patients are in side-rooms, apparently close to death. One man has his family around him, huddled in silence. In another room an elderly woman is staring motionless at the ceiling, her daughter in a chair at her side, looking anxiously out at anyone who passes the door.
“One person died last week, and this week we will probably have four. Rehab should mean that we have patients who are more stable than that,” Melton says. “I think that the patients are sicker possibly because the acute stroke wards are under pressure to free up beds. We tend to get them earlier, before they are stable. They shouldn’t be dying here. We are a rehab unit, which would usually indicate that they are going to get better.”
Pressure from job cuts
Staff have not yet fully felt the impact of the looming job cuts, but they have noticed that a new policy to ensure that physiotherapists and occupational therapists are available to patients seven days a week has had the effect of reducing their availability during the week, since no new therapists have been appointed to fill the gaps.
One of the nurses specialising in complex discharge – responsible for making sure that adequate preparation has been made for patients to go home – says staff have been cut in her department already, so she has had to cut the time she spends with patients.
Despite the new policy to move people on fast, the nurse, who asks not to be named, still finds it difficult to get all the permission in place, and to find a suitable place for them to go. Partly this is because patients’ relatives have become much more demanding over the past two decades, she says, and many are less willing to give up their jobs to look after their parents.
“Public expectations are very high. People say, ‘You can’t send my parent home until they are better,’ but quite often they haven’t been well for years. If you find an empty bed on any of the wards, it will have someone’s name on it. There are never empty beds anywhere. You can’t get people off the wards, there is nowhere for people to go.” She is also conscious of how cuts to social services mean that “re-enablement programmes” that used to be available to help patients settle back at home are no longer on offer.
The hospital is constantly introducing clever initiatives to improve treatment, which have the side-effect of saving money. New systems have been introduced to stop people being admitted when they could be treated at home. An elderly care consultant works full time in A&E, to make sure people with less serious complaints are not admitted. A day clinic has been opened to treat elderly inpatients with routine conditions, so that they don’t occupy a bed. The hip fracture service has been redesigned, so that the average stay of 35 days for these patients is gradually being reduced.
Bridget Leach, a senior nurse and a falls consultant, makes her way around the hospital, talking to elderly patients and recommending changes in their drug levels that might make them less prone to falling. “One person every four hours dies from having a fall. It’s a misconception that when people hit 65 they start to fall over randomly – there are a whole lot of reasons why somebody might fall, and a whole lot of things we can do to prevent it from happening. A hip fracture costs around £13,000. If we can stop that, it’s money saved,” she says.
She spends 20 minutes talking to Ronald, 91, recently admitted because he fell down in the night on his way to the loo, hit his head, lost consciousness and lay on the bathroom floor until he was found by a carer. He tells her he doesn’t like to wear his alarm beeper all night in case he rolls on it and sets it off accidentally. She recommends some physiotherapy and a reduction in his drug intake to minimise dizziness.
The challenges of dementia
A man with dementia has wandered to the centre of the ward where he is fiddling with the nurses’ trolley, piled up with paper folders of medical records. A younger man, lying on his back with his eyes shut, naked legs poking out from under a sheet, shouts at him without opening his eyes. “Don’t touch that!”
A nurse comes to tell the man with dementia that he has visitors and he waves his arms angrily and says: “I don’t care who comes here, I’m not performing again . . . blowing balloons out again.” His youngish daughter looks embarrassed and distressed.
“Are you all right?”
“No, I’m not all right.”
He drifts to the other side of the ward and starts fumbling at the fire escape door that doesn’t open.
“Where are you going, Bert?” a nurse calls from the other side of the room.
“I’m going to the toilet,” he says, cross and frustrated.
“It’s this one, Bert,” she says, sounding exhausted and impatient.
Medical staff have to work hard at transforming the way they operate to care for the increasing number of people with dementia, and treating patients who have dementia, alongside the conditions for which they have been hospitalised, adds an extra layer of responsibility for staff.
Chief executive Newbold is confident that the financial challenge can be met and conditions improved for patients at the same time. “What is the No 1 priority of the health service? It has to be care of the frail elderly. It’s much too hospital-based. There are thousands of beds that are needed because the model of care for the frail elderly is wrong,” he says.
“When the NHS was set up 60 years ago, it was set up to deal with people who were well, who got ill, and who went to hospital, where you treated them until they were better. Over the last 60-odd years, we’ve seen an ageing population and a massive rise in the number of people with basically incurable long-term conditions: chronic emphysema, bronchitis, chronic heart failure, arthritis.” Slowly hospitals are trying to redesign themselves and change perceptions, so that patients don’t come in for long stays with these complaints, he says.
“I’m not trying to say it is easy; it is really challenging. But I’m not going to sit here and make cuts to services to meet a budget when there are obvious changes that save far more money, and will improve the care model. That’s what we have to concentrate on.”
In his shabby office, Kamalarajan remains worried about the scale of the changes required. “I am very anxious. There is a squeeze on the available resources for the department, so that my anxiety is that I will not be able to meet the needs of the patients who need to come into hospital. That is my fear . . . patients who need to be with us,” he says. He is unhappy at what we he feels is a broken commitment from the government.
“David Cameron said he would ring-fence the NHS. We don’t feel that is what is happening.”
All patient names have been changed, and photographs do not relate to the cases mentioned in this article.
• On Wednesday, in the final part of our special report, Amelia Gentleman looks at how Heartlands A&E department is stretched to breaking point.
guardian.co.uk © Guardian News & Media Limited 2010
Published via the Guardian News Feed plugin for WordPress.
One response
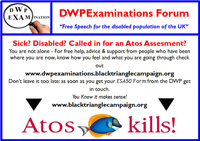
With no hope of the authorities looking after people at home, the cuts are killing elderly and disabled people!